I never knew my aunt, Pessimindle. As a teenager in the early 1900s, she developed appendicitis and rapidly succumbed to the infection. At the time, there were no antibiotics. When I was growing up, my father contrasted the loss of his sister with the advent of penicillin that saved many of his fellow soldiers in the waning days of World War II. I was taught that medicine could create miracles, which should never be taken for granted.
Penicillin was serendipitously discovered when the researcher Alexander Fleming went on vacation in the summer of 1928. He returned to his laboratory at St. Mary’s Hospital, London, to find that a petri dish with bacteria had been left open and had become contaminated by a relatively rare strain of airborne mold, Penicillium notatum, its spores likely drifting in through the window. The growth of the bacteria in the dish was inhibited by the mold. Its inhibitory substance, termed penicillin, was produced in scant quantities and was laborious to purify. A worldwide search was launched to find other strains of Penicillium that produced higher concentrations; promising samples were obtained in Cape Town, Mumbai, and Chongqing, but the best came from an overripe melon bought at a fruit market in Peoria. Pharmaceutical companies scaled up production of the antibiotic and, beginning with the D-Day landings in 1944, it was widely available to Allied troops.
Fleming recognized not only the opportunity afforded by the open petri dish, but also the peril from misusing the drug. In his speech accepting the 1945 Nobel Prize in Physiology or Medicine he said:
The time may come when penicillin can be bought by anyone in the shops. Then there is the danger that the ignorant man may easily underdose himself and by exposing his microbes to non-lethal quantities of the drug make them resistant. Here is a hypothetical illustration. Mr. X has a sore throat. He buys some penicillin and gives himself, not enough to kill the streptococci but enough to educate them to resist penicillin. He then infects his wife. Mrs. X gets pneumonia and is treated with penicillin. As the streptococci are now resistant to penicillin the treatment fails. Mrs. X dies. Who is primarily responsible for Mrs. X’s death? Why Mr. X, whose negligent use of penicillin changed the nature of the microbe. Moral: If you use penicillin, use enough.
Fleming’s advice to use the antibiotic properly was widely disregarded, not by “the ignorant man” but by “negligent” medical professionals. Prescriptions of penicillin in suboptimal dosages led to the emergence of bacteria resistant to it.
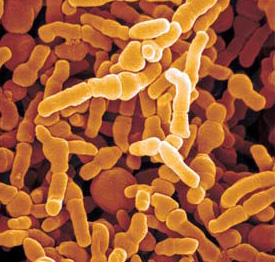
This is because bacteria reproduce at an astonishing rate. E. coli, commonly found in our colon, has a generational interval of about twenty minutes. Homo sapiens has an average generational interval of thirty years. So, over two and a half years, E. coli goes through the same number of generations as we do in two million years. As DNA is copied to spawn the next generation, random errors (mutations) occur, and the more copying, the more random mutations. If an antibiotic is used in suboptimal concentrations, then bacteria with random mutations that confer some level of resistance to the drug are more likely to survive and over many generations become impervious to it.
Researchers thus play leapfrog with bacteria that are resistant to one antibiotic by searching for a new one that is effective. William Hall, Anthony McDonnell, and Jim O’Neill in their lucid and thoughtful book Superbugs recount that for several decades, this strategy succeeded. But now we are running out of options. Potent antibiotics that were mainstays in the clinic over the four decades that I’ve practiced medicine, like ampicillin, ceftazidime, and imipenem, typically fail to eradicate many of the bacteria that currently cause infections.
Bacteria that have developed immunity to a large number of antibiotics are termed “superbugs.” The best known is methicillin-resistant Staphylococcus aureus, or MRSA. It originally appeared in intensive care units, among surgical patients. In this setting, MRSA primarily causes pneumonia and bloodstream infection from catheters. But over the past two decades, the resistant microbes have spread outside hospitals to the larger community. At the end of the 1990s this superbug infected children in North Dakota and Minnesota, then was found among men who have sex with men and in prisons among prisoners. A widely publicized outbreak occurred among the St. Louis Rams football team, transmitted by shared equipment. Other MRSA outbreaks were reported among religious groups in upstate New York, Hurricane Katrina evacuees, and people who have received tattoos without proper sanitary precautions. Resistant forms of so-called gram-negative bacteria—characterized by cell walls that protect them from many antibiotics—have also emerged, like Klebsiella and Acinetobacter, which often cause death. Recently, resistant strains of gonorrhea have been detected in Asia.1
Superbugs only briefly reviews the science of bacterial resistance; its focus is on the societal consequences. While there are no exact data on the total number of people dying each year from resistant microbes, the authors calculate it to be at least 1.5 million. This number outstrips deaths from road accidents (1.2 million) and approximates the number of deaths from diabetes (1.5 million).
The economic burden on our health care systems is considerable. People with resistant infections spend more time in the hospital, require more care from doctors and nurses, are treated with more expensive drugs, and often have to be isolated from other patients. In the United States, it costs an average of $16,000 to treat a patient with Staphylococcus aureus that is susceptible to the antibiotic methicillin, with an 11.5 percent chance of death; if the bacteria are resistant, the cost jumps to $35,000 and the chance of the patient dying more than doubles. A study from the European Medicines Agency in the European Union, which includes England, estimated the cost to EU healthcare systems at €900 million ($1.06 billion)
The impact of bacterial resistance on economic productivity is also significant. The Centers for Disease Control and Prevention in the United States have estimated that resistance costs the American health care system about $20 billion per year, to which productivity losses add a further $35 billion. Using the American estimates, the authors of Superbugs extrapolate the total costs of antimicrobial resistance worldwide to about $57 billion for health systems, with the reduction in world productivity valued at $174 billion.
Based on these economic calculations, Superbugs provides a set of policy prescriptions, framed in pragmatic terms meant to motivate self-interested politicians:
Governments might not want to invest in solutions, but they will ultimately pay either way. Any money not spent now will result in substantial costs in the future—not to mention many lost lives. Serious damage to economic productivity (which by extension threatens governments’ tax incomes) coupled with the higher costs of health care (which is largely government funded) should provide the impetus to deal with this crisis now.
Investment to combat superbugs begins with identifying new antibiotics. Almost all antibiotics are still derived from natural compounds, like Fleming’s penicillin. Although researchers at the Rockefeller University have recently devised advanced methods to facilitate the search, it is unclear how many antibacterial agents are left to discover.2 The most prudent approach is to rely not on discovery but on conservation. “We need to think of our current antibiotics as nonrenewable natural resources,” Hall, McDonnell, and O’Neill write.
Long before we discovered the environmental damage caused by burning hydrocarbons, we were keenly aware that one day the world would run out of coal and oil and that not only should we not waste them, but we should develop renewable resources.
This in part has been the focus of Environmental Protection Agency (EPA) regulations:
Both government and industry plan for the exhaustion of rare earth metals that are needed in electronics and elsewhere. This is not to say that we will never find any new antibacterial compounds…. However as it is unclear how many more drugs can be found in the future, we should work hard to protect the ones we have, as well as new ones that we find.
They provide a concise overview of the logistics of new drug development. It normally takes ten to fifteen years to bring a new therapy to market, at a cost of more than a billion dollars. Intellectual property rights give the company a monopoly over the drug for some twenty years, depending on the country. After that, low-cost generic manufacturers typically jump in to sell it at a reduced price. Much of those twenty years is spent testing the drug in clinical trials, so investment costs are recouped over only about a decade. The company generally makes no significant profit after the patent expires. Still, high sales usually mean that patented drugs end up making a profit.
Antibiotics, the authors show, are paradoxically different in the marketplace when properly prescribed:
If an excellent new antibiotic is effective against infections caused by drug-resistant bacteria, most public health officials would want to protect it for use in the most extreme circumstances and would discourage it from being sold worldwide. To get the maximum benefit from the drug and prevent the development of resistance, it is important that people not use it frequently.
This makes eminent sense from a public health point of view, in effect safeguarding a precious social resource:
When asked what she would do with a useful new antibiotic, the chief medical officer for England, Sally Davis, said that the drug “would need a stewardship program”—that is, that systems would have to be in place to make sure that the antibiotic was only prescribed when absolutely necessary. Indeed, limiting unnecessary use is essential to keep bacteria from becoming resistant to new antibiotics, and thus essential for our continued health.
While this is a cogent strategy, it doesn’t coincide with the marketing goals of the drug industry: “When a really useful new antibiotic is found, the company that invests in it cannot rely on high sales for return on investment.”
Commercial imperatives also work against societal needs in the use of antibiotics in animal husbandry. This is partly a result of the sheer number of animals being reared yearly to feed the world’s seven billion–plus people. Antibiotics were introduced into agriculture in the 1950s, when it was discovered that regular low doses of them made farm animals grow faster and larger. Consumers could purchase meat at lower prices, since the drugs reduce production costs for farmers. Globally, more antibiotics are estimated to be used today for animals than for humans. For example, “over 70 percent of medically important antibiotics in the United States, by volume, are sold for use in farm animals.” Hall, McDonnell, and O’Neill note that
antibiotics are more effective growth promoters when used for animals kept in cramped, dirty, unregulated conditions than for animals living in cleaner, more open, more controlled environments. Under suboptimal conditions, the growth promoters are for all practical purposes a substitute for good infection prevention and control.
The effects of antibiotics on growth are not fully understood. They may alter the animal’s microbiome—the bacteria in the gut—as well as prevent infection, so less energy is expended on fighting microbes.
Our environment is becoming contaminated with antibiotics and their residues in several ways. The first is a result of body waste—from both animals and humans. According to Hall, McDonnell, and O’Neill, “Studies suggest that as much as 75 to 90 percent of antibiotics may be excreted from animals without being metabolized. This waste goes into the soil and is then washed into the water systems.” Second, when pharmaceutical factories dump their untreated waste that contains the active ingredients of antibiotics into the water supply, they save money on expensive disposal. Such practices encourage the development of antibiotic resistance, since we are thus exposed to low and varying amounts of the drugs, as Fleming warned.
Hall, McDonnell, and O’Neill argue that “antibiotics provide a backbone to the entire healthcare system,” essential in everything from hip surgery to cancer treatment to organ transplantation. Thus developing effective antibiotics should be recognized as a “public good.” This justifies governmental intervention with incentives for the creation of new drugs. But such incentives have not been forthcoming, partly, in the authors’ view, because “electoral cycles encourage short-term thinking.” This kind of thinking has become particularly acute with the economic and social upheavals of the recent elections in the United States and Europe:
If a prime minister or president invests government resources to curtail drug resistance, they are unlikely to get huge rewards from the electorate. People generally do not vote on how well the government is dealing with a future problem, and they do not have enough knowledge of the early stages of research to make judgments. As a result, the political incentives have not been sufficient to pressure governments into action.
To overcome these barriers, they recommend a public innovation fund that covers early-stage research, as well as “non-cutting edge research that has societal benefit but little commercial attractiveness”; enhanced collaboration among companies in conducting clinical trials; harmonization of new drug regulation to reduce the costs of development; and “market entry rewards” that will compensate a company for creating useful products.
In agriculture, the authors write, methods are needed to rear animals without antibiotics. But “progress on an international scale will be a challenge because many meat-producing countries have a financial interest to continue antibiotic use.” Still, farming practices can be profitably improved, as occurred in Denmark, where farmers significantly reduced use of antibiotics while sustaining productivity; the country is one of the largest exporters of pork in the world. This has been possible despite regulations to limit the use of antibiotics, in part because of improved infection control procedures, which lowered infection rates and reduced the need for drugs. Denmark also improved the monitoring of antibiotic sales and use, which enabled the government to intervene if farmers were disregarding the law. It did this through what was called a “‘yellow card system’—pig farmers using the most antibiotics were sent warnings that they might face penalties.”
Given this evidence of economic competitiveness despite the regulation of antibiotic use in livestock, Hall, McDonnell, and O’Neill propose international agreements as a first step toward remedying the urgent issue of superbugs. “A combination of taxation, regulation, and subsidies for alternatives to antibiotics should be developed.”
But regulation is needed not only in farming. When we are treated for bacterial infection, we excrete unmetabolized antibiotics that enter our water systems. As the authors write, “A wastewater system that eradicates all traces of antibiotics does not yet exist, partly due to the high cost of development.” This issue is especially prominent in hospital waste, since patients are more likely to have antibiotic residues in their feces, in addition to drug-resistant bacteria. “This combination has the potential to create hotspots of resistance.”
Yet another obstacle is found where antibiotics are often manufactured, in India and China, where production costs are minimal. There is often poor quality control of the content of the antibiotic pills manufactured in these countries. They also often contain less of the active drug than advertised.3 Again, as Fleming noted, undertreatment with suboptimal doses of antibiotics fosters bacterial resistance.
At the 2016 G7 meeting, chaired by Japan, world leaders recognized how market forces mitigate against new drug development and called on international institutions to rectify the problem. While these leaders recognized the importance of increased access to antibiotics for their underserved populations, they also highlighted the need for stewardship in use of the drugs for both patients and animal husbandry.
The authors assert that political will is needed to find the funds for implementing incentives. They estimate that an investment of $40 billion over ten years is required for the world to avoid a $100 trillion cost by 2050. They argue that “the potential to prevent an increase from 1.5 million to 10 million deaths per year should make every one of us stand up and take note.”
But I am not hopeful that such pragmatism will prevail. Superbugs was written before the sharp shift in our politics, notably Brexit and the election of Donald Trump. The withdrawal of the United States from both the Paris Climate Accord and the Trans-Pacific Partnership has been followed by a declaration of trade wars, which the president tweets are “good” and “easy to win.” This absurd delusion fits with his view that all deals are binary, with “winners and losers” rather than agreements that may benefit both parties in the negotiation.
Such brute nativist thinking undermines global cooperation, which is needed for the proposals of Hall, McDonnell, and O’Neill. If the recent lifting of salutary regulations by Trump’s EPA on the chemical and mining sectors are any indications of disregard for the environment, there is scant hope that measures to limit factory dumping of antibiotic waste will be pursued. Still, some within the administration are trying to address the threat of superbugs in the defense budget, where research on antibiotic resistance may be cloaked under the aegis of national security.4 But such singular measures will ultimately fall short without a comprehensive and coordinated plan of cooperation among nations.
 Campaign Poster
Campaign Poster Campaign Poster
Campaign Poster
:format(webp)/cdn.vox-cdn.com/uploads/chorus_image/image/60199985/Foto_7.0.jpg)
:format(webp)/cdn.vox-cdn.com/uploads/chorus_asset/file/11602219/Screen_Shot_2018_06_26_at_8.26.12_PM.png)