By Michael Friedman, Monthly Review, July 1, 2018
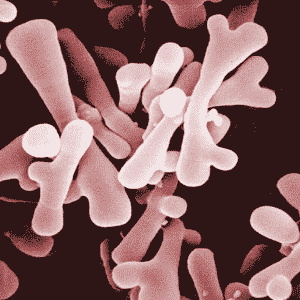 |
| Bifidobacterium via Wikipedia Commons. |
Metabolic rift theory has been applied to understanding various instances of our society’s disruption of ecological processes. Capitalism, with its ever-expanding production to realize profits on an ever-growing market has created innumerable rifts between natural and social “metabolic” processes. Both as an analytical approach and a metaphor, metabolic rift theory also sheds light on the forms of disruption of human microbial ecosystems, with consequences for human health. Human microbiota, comprised of the microorganisms living on and in humans, has been shown to be essential for a growing list of physiological, metabolic, and developmental processes, as well as to mediate between environmental and physiological processes. Alterations of microbial biodiversity that result in disruption of microbial ecosystem functions (collectively referred to as dysbioses), have been associated with many noncommunicable and autoimmune conditions that are increasingly prevalent in industrialized and developing nations. Major factors favoring these dysbioses include diets high in processed foods and extensive antibiotic exposures.
These factors cannot be divorced from the practices of respective industries that see profits and capital accumulation as their primary goals. These goals favor production that is divorced from ecological networks and respond to a reductionist paradigm that conceives of complex processes in terms of simplified causal chains. Capitalist production results in cascades of unforeseeable consequences, which must then be met by magic-bullet solutions, setting the stage for further undesirable consequences. While practical health measures arising from emerging knowledge of the microbiome are important, they do not address the underlying cause of the disruptions that cause dysbioses. We can expect to continue to see disruptions of the microbiome until we are able to re-conceptualize and transform our engagement with ecosystems large and small, and with the assistance they provide to humankind.
“Metabolic rift” is the concept popularized by environmental sociologist John Bellamy Foster, following Marx and others, to describe the disruption of ecological processes and the tendency to sever the connection between ecological and social realms.1 Foster attributes the metabolic rift to the intrinsic dynamic of capitalist production, with its private ownership of the means of production, drive for profits, ever-expanding markets, and continuous growth. Marx employed this idea to describe the effects of capitalist agriculture on the degradation of soil fertility. Foster and his co-thinkers have employed the concept in analyses of climate change, biodiversity, agriculture, fisheries, and many other aspects of human interaction with our biosphere.2
There is perhaps no more appropriate use of this concept than in reference to the microbial ecosystems of which we are a part, and which are part of us—the human microbiota, organisms living on and inside of humans—and the disruptive impact the prevailing mode of production and consumption has had on them, with serious consequences for our health.
Our Own Ecosystem
Over the past decade and a half, advances in DNA sequencing technology and bioinformatics, as well as theoretical advances in other areas of science, particularly ecology, have favored paradigm-shifting research on what is popularly called the human microbiome. In the literature, “microbiota” is generally used to denote the totality of microbial communities inhabiting different body regions, and includes bacteria and viruses, as well as eukaryotes (organisms with nuclei), such as fungi and amoebas. The microbiome refers to the collective genomes of these organisms. Biologists are now able to sample the genomes of entire microbial communities, particularly those living on and in us, allowing us to identify many thousands of new microorganisms, which had previously been unknown largely because they did not grow on culture dishes.3
Based on this research, together with subsequent progress in identifying key genes and their products, as well as metabolic pathways and metabolic byproducts, researchers have identified a host of vital functions and networks involving these microbial communities and their hosts. Informed by ecology, investigators of human microbiota realized that they were looking at entire ecosystems, of which we are but one (albeit crucial) species.4
Our body ecosystems are integrated by a high degree of mutual dependency, the result of millions of years of coevolution. For example, a primary function of maternal milk, beyond infant nourishment, is the formation and development of the immune system of infants. Breast milk contains a vast, species-specific array of relatively small bioactive carbohydrates (human milk oligosaccharides), indigestible to human babies but accessible to bacterial enzymes. A single variety of bacterium called Bifidobacterium longum infantis has coevolved with Homo sapiens from related bacteria in our primate ancestors.5 This bacterium contains all the enzymes necessary to process these carbohydrates.6 It is a critical early colonizer of the human gut, and is involved in various aspects of infant nutrition and organ system development.7
There are approximately as many microbial as human cells in our bodies.8 Our gut microbiomes alone consist of up to a hundred times more distinct genes than those possessed by our own cells and perform a host of metabolic functions of which our cells are incapable.9Several distinct microbial ecosystems cohabit our bodies. These are characteristically found in our oral cavity, respiratory, gastrointestinal and vaginal tracts, and our skin. The largest, most complex and best-studied microbial communities form the gut microbiome. This comprises some 39 trillion bacterial cells (and large numbers of other organisms).10 Many of these microscopic symbionts, living in a mutually beneficial relationship with humans, are integrated with our body systems through intricate food webs. Some bacteria consume the metabolic products of other bacteria, and so on down the chain, finally producing small molecules that have important effects on human physiology.11 Some bacteria and their cell components engage more directly with our cells, while others engage in forms of competition, predation, and other interactions with other microbes.12 Some biologists conceive of our microbiota as a hitherto unrecognized organ or organs fulfilling important physiological functions and networking with other organ systems, while many microbial ecologists propose that we are not “individuals,” but collective organisms comprised of the person (mammal) and its entire microbiome. Many other species are also collective organisms, termed holobionts, tightly bound by evolution ever since the earliest eukaryotic cells arose from fusions of independent prokaryotes (non-nucleated cells, such as bacteria).13
Accustomed to seeing microbes as deadly enemies subject to a “war on disease,” scientists and health professionals have begun rethinking the microbiota as essential components of our health, and indeed our development and evolution. Many disease states are being reconceived as the result of disruptions of normal ecological states caused by changes in microbiological diversity in the same way that alterations or loss of biodiversity can give rise to susceptibility to invasion, decreased community productivity and ability to adapt to change, and loss of other ecological functions and services.14 Just as monocrop farming systems favor proliferation of pests, facilitated by evolved resistance to pesticides, changes in gut biodiversity as a result of antibiotic use seems to favor invasion by pathogens, such as the often deadly gastrointestinal pathogen Clostridium difficile.15
Like other ecosystems, our microbial ecosystems develop from colonization through a series of successions, with each stage contingent on previous ones. And like forest ecosystems, for example, disruption of early stages can have far-reaching consequences for the host and ecosystem.16 If a cleared field is subject to ongoing disturbance, normal stages of succession will not occur. Instead, the field will be colonized by an assortment of opportunistic species. Something similar happens when the natural process of colonization and normal successional stages of microbiota are disrupted.17 Studies have confirmed that successional states of babies’ microbiota can be retarded and loss of function can occur following disturbance at early stages.18
Some evidence suggests that our bodies are initially colonized in utero via the placenta and amniotic fluid.19 Most studies confirm that the major surge of colonization occurs at childbirth, as the baby passes through its mother’s birth canal. This initial microbiota comes from the mother’s vagina.20 Another major microbial succession develops through breast-feeding, with colonizers like B. infantis possibly introduced through the milk and/or proliferating from populations already present pre- or post-partum on the basis of milk carbohydrates.21 These initial successions are critical to our future health. They are involved in the formation and development of a number of body systems.22 Initial, healthy microbial communities are not established in cases of pre-term births, caesarian sections, or formula feeding. Normally, our microbiota assume an adult configuration by about five years of age, although they continue developing through adolescence.
While there are certain taxonomic commonalities at given successional stages at given body sites among different individuals, individual hosts vary greatly in terms of microbial species. Yet core sets of major taxonomic groupings and metabolic functions seem to be conserved across individuals at given body sites, absent disruption. As is the case with macro-ecosystems, healthy microbial communities possess a high degree of functional redundancy: various, even unrelated, bacteria fulfill the same functions, and fill the same metabolic “niches” in different individuals.23 This functional redundancy is facilitated by horizontal gene transfer from one organism to another (unfortunately, including pathogenic genes) as well as by convergent evolution.24 And such redundancy enables microbial communities to restore or retain metabolic functionality following disturbances, ecological properties known as resilience and resistance. But it is not infallible in the face of systematic ecological disturbance and biodiversity loss, which can compound across generations, which is what we seem to be experiencing at both macro and micro levels in our industrialized and industrializing societies.25
Microbiota-Physiological Interactions
The human microbiota engages in interactions with all body systems in which both the body and microbiota benefit (a “mutualistic” relationship), often as critical modulators of developmental, metabolic, and physiological functions, including roles in the formation of the vascular system, formation of bone tissue, and brain and neural development and modulation.26
The most important roles of microbial interaction involve development and modulation of the immune system. Recent microbiome research has reframed our understanding of the very role of the immune system from a defensive bastion to a gardener, cultivating a healthy microbiota.27 Symbiotic microbes, especially in the gut, are thought to play crucial roles in mediating the body’s critical inflammatory response. Inflammation is vital for coping with pathogens and antigens; its dysfunction is implicated in a host of chronic metabolic and autoimmune diseases epidemic in modern societies. One set of mechanisms involves bacterial regulation of the balance between immune system cell types.28 This mediation may be carried out by way of various products of bacterial metabolism, such as short-chained fatty acids. The equilibrium between pro- and anti-inflammatory immune functions may be disrupted by various environmental inputs, including diet and antibiotics, via alterations to the microbiota. In turn, changes and breakdowns in microbial communities have been linked to several chronic and pathogenic disease states, such as allergies, asthma, and inflammatory bowel disease.29 Symbiotic microbes also play more direct roles in blocking pathogen colonization, by outcompeting or destroying them.30
Interactions between the microbiota and the digestive system are among the earliest and best known. Beyond producing human nutrients through vitamin synthesis and breakdown of complex carbohydrates, gut microbiota play a mediating role in carbohydrate and lipid uptake, storage, and metabolism. They do this through metabolic products and secretions that allow them to interact with the intestinal lining, adipose cells in body fat deposits, and cells in the liver, including cells which produce the “hunger hormones,” leptin and ghrelin.31 They also play a critical role in the development of the child’s intestinal lining and mucosa, including growth of the finger-like villi vital for nutrient absorption, and the intestinal vascular tissue.32
The gut microbiota is also believed to play a role in nervous system development and function. According to Stephen M. Collins and others, various mouse studies indicate that the microbiota affects “the development of neuronal circuitry that is relevant to a broad spectrum of activities, including anxiety-like behavior, motor control, memory and learning.”33
Bacteria mediate a series of pathways known as the “gut-brain axis.” This axis involves biochemical cross-talk between the dense complex of neurons associated with the gastrointestinal tract, the vagus nerve, the neuro-endocrine and immune systems, and the brain.34 It is a two-way superhighway, which not only affects digestive and immune functions, including secretion of pro-inflammatory substances, but also affects mood and behavior. The Hypothalamus-Pituitary-Adrenal axis (HPA), which regulates the stress response, is one component of this “gut-brain axis.” A number of gut microbes are known to enhance or suppress the release of stress hormones by the HPA axis.35
In addition, the microbiota can interact via other mechanisms with various regions of the brain, including the emotion-regulating limbic system, possibly through products formed by the workings of cells (metabolites), such as lactic acid, or through secretion of known neurotransmitters, such as acetylcholine or GABA.36 Microbial metabolites and cell products also impinge on the vagus nerve and enteric nervous system.37 Microbiota-induced changes in immune system function can also affect neurological function through pro- or anti-inflammatory mechanisms.38 Shifts in bacterial communities may factor into a number of mental disorders, including depression, autism, and schizophrenia.39
Our bacterial communities are important modulators of our energy metabolism, operating through various mechanisms, such as direct interactions with intestinal cells or stimulation of neuroendocrine or inflammatory pathways. Distinct microbial communities can either facilitate energy uptake and storage as fat, or efficient use of energy sources by muscle and other cells. Thus, different microbial communities are associated with types of obesity and overweight, as well as the suite of disorders related to the metabolic syndrome. In particular, some microbial suites are thought to favor insulin resistance, a pivotal condition of metabolic syndrome, associated with type 2 diabetes and cardiovascular disease, during which both serum insulin and glucose levels increase, as muscle and other cells cease taking up glucose in response to the insulin. Early studies showed that transfer of microbial communities from overweight humans to germ-free mice fed lean diets can induce obesity and fat storage in the mice. In contrast, germ-free mice fed high-sugar and high-fat diets showed resistance to obesity. Moreover, in both humans and mice, gastric bypass surgery (RYGB) shifts microbiota from obesity-associated states to lean-associated states. What is more, when these gastric bypass microbiota are introduced into germ-free mice, they show reductions of serum triglycerides and body weight. As Kristina B. Martinez and colleagues explained, “taken together these data suggest that the microbiota following RYGB in humans and mouse models elicits a direct functional impact on host energy balance, resulting in restoration of metabolic homeostasis and resistance to diet-induced obesity.”40
Microbiota Disruption and Disease
In macro-ecosystems, persistent disturbance can compound and lead to state changes in the ecosystem, shifts in species and populations of organisms and ecosystem functions.41Biodiversity decline can lead to the loss of ecosystem functions and services, such as productivity, nutrient cycling, resilience, and resistance to invasion.42 This is why monocrop farming is particularly prone to pests, for example. Ecosystem functions constitute the “metabolism” of a community. The loss of ecosystem functions and services is due to the loss of both redundant and complementary functions of organisms.43 For example, pesticide use can result in loss of beneficial predatory insects and pollinators or nitrogen-fixing symbiotic bacteria.
Just as is the case in macro-ecosystems, the microbiota shows a degree of resilience in the face of stressors. However, dramatic or persistent stressors can induce changes from healthy community composition and functionality to degraded communities (dysbiotic states), or can even cause the collapse of the microbial communities.44 Moreover, previously adaptive states might be rendered maladaptive under altered environmental conditions.45 These appear to be occurring at present, particularly in industrialized societies, but increasingly in developing nations. Residents of industrialized societies show reduced microbial biodiversity compared to members of agrarian or hunter-gatherer societies, as well as a shift to bacterial communities with enhanced energy storage functions—production of metabolites that favor inflammation and other manifestations of a rift between symbiont-host relationships.46 At the same time, global societies are in the throes of an epidemic of non-communicable, chronic, and autoimmune diseases that have been linked to the “western lifestyle.” Moreover, these diseases show a socioeconomic gradient.47 Industrializing societies increasingly present these same dysbiotic states, while continuing to manifest other dysbioses associated with malnutrition.48
Two related theories, both supported by experimental and epidemiological data, may help explain these observations. The better-known of the two, the “hygiene hypothesis,” affirms that lack of childhood exposure to microbes limits normal development of the immune system and leads to susceptibility to allergic and autoimmune conditions.49 The second, known as the “disappearing microbiome” (or more generally, biodiversity) hypothesis, links social and environmental factors such as diet, rampant antibiotic use, and current medical practice to the loss of microbial biodiversity and ecosystem functionality.50 One recent study demonstrated that a diet low in fiber and high in fat and protein produced a decline in gut microbial diversity that compounded across generations.51 Nor could these losses be corrected simply by restoring high-fiber diets to experimental subjects, indicating that some deficiencies were permanent, barring benefits from transplants of microbiota.52
Microbial community disruptions have been associated with a growing number of both pathogenic and non-communicable illnesses. These include metabolic syndrome (discussed above), as well as Irritable Bowel Syndrome, Inflammatory Bowel Disease, necrotizing colitis, asthma, Kwashiorkor, Parkinson’s Disease, allergies, various types of cancer, Autism Spectrum Disorder, multiple sclerosis, chronic depression, dermatitis, periodontal disease, and candidiasis, among others.53
Environmental Impacts on Microbiota
Many factors shape the development and functioning of the human microbiome. However, two seem to play inordinately important roles in shaping community composition and inducing dysbioses: host nutrition and exposure to antimicrobials and other pharmaceutical compounds.
Diet
Diet and dietary change are thought to have the single greatest impact on our gut and possibly all other microbiota, as a result of both nutrient availability and the effect of what we consume on local environmental conditions, such as pH, secretion of bile, and so on. Studies on the coevolution of mammals and intestinal microbial communities have shown that characteristic microbiotas are associated with herbivorous, carnivorous, or omnivorous hosts, independent of host taxonomic group. And humans favoring herbivorous or carnivorous diets possess microbiota similar to other mammals that rely on these diets.54
Gut communities differ strongly between individuals who consume diets high in simple sugars, animal fats, and processed foods—i.e., the “Western diet” or “industrialized diet,” and consumers of diets rich in vegetable fiber and other complex carbohydrates, sources of vegetable protein and fish.55 People consuming diets rich in fiber have greater diversity of gut microorganisms, reflected in greater diversity of genes and functions of microorganisms.56Such diets favor a preponderance of types of organisms (taxa) and functions associated with production of a number of beneficial metabolites and favorable interactions with our immune and other systems.57 Diets rich in certain fats and simple sugars, in contrast, are associated with diminished diversity at various levels, seem to favor taxa that support greater energy extraction and storage functions, and tend to produce a number of harmful metabolites that favor inflammation.58
Short-term dietary variations can produce alterations to the microbiota. Generally, a healthy, resilient microbial community can rebound from such disturbance. Consecutive short-term changes and long-term dietary shifts can have profound, continuing, even permanent impact on the microbiota.59 Studies directly comparing diets provided over different durations indicate that long-term consumption of the Western-type diet favors distinct microbiota types with functions associated with detrimental health outcomes.60
Marit Zinöcker and Inge Lindseth argue that “the Western diet promotes inflammation that arises from both structural and behavioral changes in the resident microbiome. The environment created in the gut by ultra-processed foods, a hallmark of the Western diet, is an evolutionarily unique selection ground for microbes that can promote diverse forms of inflammatory disease.”61 They then point to a large number of studies linking food additives—including emulsifiers and artificial sweeteners, low fiber content, high fat and sugar content, and chemical byproducts of food processing—to both shifts in bacterial communities and inflammation.
High-fat diets and specific fat types have been linked to alterations of the microbiota and various metabolic markers. Research by Lawrence David and colleagues demonstrated that shifting from a diet rich in vegetable fiber to one based on animal fats produced a dramatic change in human gut community structure and functionality, with a decrease in beneficial classes of bacteria and bacterial metabolites and concomitant increases in detrimental bacteria and gene products.62 A similar study on mice also pointed to the overwhelming impact of high-sugar/high-fat (saturated animal fat) diet on microbiota.63 Studies comparing omega-6 polyunsaturated (vegetable) fats with animal-based saturated fats, and omega-3 rich polyunsaturated fish oils, showed different bacterial groupings and functions in the experimental mice, which, in turn, correlated with physiological changes in the animals. The first was associated with inflammation of fat tissue, the second with factors leading to colitis, and the third with reduced adipose-related inflammation.64 Another study indicated that diets rich in omega-3 polyunsaturated fatty acids favored enhanced neurobehavioral development in mice “closely associated with comprehensive alterations in gut microbiota composition” and other factors.65 Recent research also demonstrated bacterially mediated reduction of metabolic syndrome in mice given omega-3 fatty acids, and provided a possible mechanism for this in microbially mediated anti-inflammatory signaling.66
Simple sugar consumption is implicated in both microbial community alterations and metabolic syndrome. Work in Yael Nobel’s laboratory showed that simulated soft drink sugar combinations significantly altered the gut microbiome in infant and juvenile rats, favoring some groups associated with type 2 diabetes and reducing groups associated with beneficial bacterial metabolites.67 Another study found that a diet enriched with fructose induced symptoms of metabolic syndrome in rats, including insulin resistance, elevated plasma lipid levels, glucose intolerance, and inflammation.68 When the animals given this high-fructose diet were treated with antibiotics, microbial community composition shifted and metabolic syndrome markers disappeared. This suggests a mediating role for these groups in fructose-induced metabolic syndrome. Research by Fang Liu and her laboratory found that a seaweed-derived antioxidant reduced obesity, metabolic syndrome, and inflammation in mice on high-fat and sucrose diets, and tracked these ameliorative effects to alterations in the gut microbiota.69
In a review of existing research, Benoit Chassaing and colleagues attributed a dominant role in the proliferation of inflammatory metabolic syndrome disorders to the loss of fiber from our diets, noting that it is “the macronutrient whose levels have changed most” since the 1950s.70 A recent investigation by a member of Chaissaing’s lab found that the soluble fiber inulin suppressed metabolic syndrome in mice given high-fat diets, and delineated the mechanism involved, which was disruption of the gut microbiota by the high-fat diet, consequent loss of a protective layer in the small intestine, and infiltration of the intestinal lining by bacteria, producing systemic inflammation.71 The inulin restored the microbes and protective layer.
The global population confronts a nutritional dichotomy. While industrialized nations appear to suffer from epidemics of obesity and associated disorders, a large portion of the world’s population faces malnutrition and hunger. Both manifestations are associated with alterations to the microbiota.
While malnutrition is unequivocally due to insufficient uptake of nutrients, it can alter the microbiota, which, in turn, may mediate a number of malnutrition-related conditions or further hinder nutrient absorption. Several studies have shown that malnutrition reduces and restructures microbial diversity, and has a particular impact on bacterial communities during the postnatal period.72 In turn, this altered microbiota has been found to have a causal role in conditions like Kwashiorkor, a type of protein deficiency associated with severe malnutrition.73A series of studies conducted in Bangladesh, Malawi, and several other countries, based on clinical data as well as mouse and pig models, found that both diet and microbiota influence growth in body mass and height, affect the ability to metabolize various nutrients, and influence susceptibility to pathogens in infants.74 One key element in this equation is the familiar presence in maternal milk of human milk oligosaccharides. Researchers in Malawi and Bangladesh found low levels of these human milk oligosaccharides in breast milk of mothers with severely stunted six-month-old children as compared with healthy children.75
Researchers transferred fecal microbiota from growth-stunted children and normal children to germ-free mice and piglets. These studies showed that severe malnutrition hinders normal microbial community successions, producing immature gut microbiota with respect to the age of the child. This, in turn, was associated with reduced growth rates in children.76
In another set of studies, germ-free mice were given microbiota from either healthy or stunted human infants and then mixed together. Mice are coprophagous, meaning that gut bacteria are shared through ingestion of feces. The age-normal microbes spread to the mice with immature microbiota, ameliorating the growth-stunting effect, as compared with control mice that were just given the immature microbiota. Researchers examined the mechanisms involved in these effects and found that the gut organisms can modulate the response to growth hormone.77
Finally, researchers used targeted antibodies to identify pathogenic strains of bacteria from severely malnourished children that weakened the intestinal lining, permitting infection and producing inflammation. These pathogens, normally inhibited by a healthy microbiota, could be temporarily blocked by transplanted microbiota from healthy hosts.78
In summary, diet plays a profound role in shaping human microbial communities. At the same time, our “industrial diet,” with its emphasis on cheap, processed foods consisting of low fiber, high salt, fat, sugar, and chemical additive ingredients, has increasingly been associated with a host of chronic and non-communicable conditions epidemic in industrialized countries and increasingly sweeping developing countries. And of course the apparent opposite of this surfeit of cheap, industrial food—the absolute lack of nutrients endemic to many regions of the world—also produces pathological health issues. Numerous studies indicate that these dual forms of malnutrition disrupt the gut microbiota. And considerable evidence is accumulating, particular in the case of the “Western diet,” that this disruption is playing a causal role in that epidemic.
Antibiotics
Antibiotics are not human inventions, but have instead always been part of the microbial biochemical repertoire, produced by microorganisms not only to defeat competitors, but as a means of intercellular communication. Antibiotics have also undoubtedly been of enormous benefit to human health, principally for those who have had access to them. However, their market-driven proliferation has led to persistent exposures far beyond those normally experienced by microorganisms. Broad-spectrum antibiotics in particular have been favored, precisely due to their ability to control a broad range of pathogens, but these have had especially pronounced effects as both disruptors of microbiota and stimulators of antibiotic resistance.
Overuse of antibiotics on humans and farm animals has given rise, through natural selection, to antibiotic resistant pathogens, and then “superbugs,” bacteria that are resistant to several, or even all currently used antibiotics. And genes that confer resistance—together with other factors that enhance pathogenicity—are transferred, even between different bacterial species via horizontal gene transfer, converting normally minor members of the microbiota into opportunistic killers.
Martin Blaser, a leading authority in microbiome research and originator of the disappearing microbiome hypothesis, considers antibiotic use to be a “four-edged blade.”79 The first two blades are the benefits to individual and community health. The third edge is the long-predicted problem of antibiotic resistance, and the fourth is the damage antibiotics inflict on individual (and community) health through impact on the microbiota. There are many important elements to this impact.
First, although there are differences in the specific effects of different antibiotic types, in general, these drugs have been shown to alter microbial communities and their functional capabilities. In a survey of antibiotic impacts on microbiota, sixty-eight antibiotics affected abundance of forty-two major bacterial genera, some only impacting one or a few taxa, while others affected up to thirty-two genera.80 The main phyla affected include the principal phyla in the human microbiome: the Bacteroidetes, Firmicutes, Actinobacteria, and Proteobacteria. These include many important symbionts. In fact, several of the genera associated with important positive health-related functions are among the most antibiotic-sensitive types of microbes.81 Change or loss of community metabolic attributes due to antibiotic treatment can be drastic and persistent, and may result from the loss of only a few keystone taxa. Treatment by different antibiotics and combinations can result in changes in the relative abundance of bacterial metabolites in fecal samples by up to 87 percent, producing imbalances in many bioactive compounds.82 A long-term study of Finnish school children showed that administration of commonly prescribed antibiotics produced extensive losses and sharp changes in microbial taxonomic and functional composition, and correlated increases in some chronic health issues.83 The authors concluded that a major class of commonly prescribed antibiotics “may have undesired effects on the developing microbiota of children, which may compromise the development of a healthy immune system and metabolism.”
Second, many studies point to impacts of both short- and long-term administration, of both sub-therapeutic and therapeutic exposures, on our microbial ecosystems. Clinical and laboratory studies link persistent antibiotic use with enduring or permanent diversity loss, including loss of keystone taxa critical for the microbial ecosystem and human health. As a result, antibiotics may represent a major causal factor behind the “disappearing microbiome” hypothesis.84
Third, antibiotic usage also correlates with human physiological changes and a growing number of communicable and non-communicable pathologies. Studies on mice have provided evidence of causal links between antibiotic usage, alterations to the microbiota and pathologies.85 Health practitioners and researchers have long known about the phenomenon of anemia in patients given certain antibiotics. A recent mouse study showed that red blood-cell formation in the bone marrow is mediated by gut microbes via interactions with the intestinal immune system, which, in turn signals stem-cell differentiation in the marrow. Antibiotics suppress this “cross-talk” by depleting the gut microbiota.86
Fourth, as with nutrition and other factors influencing the microbiome, antibiotics appear to exercise their most profound impact during the critical developmental window during early life stages. Asthma, types 1 and 2 diabetes, obesity, celiac disease, allergies, and inflammatory bowel disease are all linked to antibiotic use via dysbioses in young children. A large cohort study of more than 28,000 mother-child pairs in Denmark found that antibiotic administration during the child’s first six months of life was associated with heightened risk of overweight at seven years of age.87
Fifth, not only does antibiotic treatment reduce biodiversity and alter community composition, but it has been shown to enhance transfer of antibiotic resistance genes between bacteria by several mechanisms. The human gut has been compared to a bioreactor, with billions of bacteria in close proximity. This means that bacteria favored with antibiotic resistance can readily transfer the respective genes to other bacteria. Antibiotics have also been shown to increase expression of bacterial genes involved in horizontal gene transfer and virus-mediated transfers of bacterial genes.
The impact of antibiotics commonly used in treatment of gastrointestinal infections is illustrative. Antibiotic administration as prophylaxis following gastrointestinal tract surgery reduces symbiotic microbes, particularly species that hold Clostridium difficile in check, resulting in loss of colonization resistance and serious infections.88 Treatment of C. difficileinfections with vancomycin, the drug of choice, also eliminates normal microbiota and favors the spread of antibiotic-resistant pathogens.89 In particular, treatment with streptomycin or vancomycin leads to infection by Salmonella strains, due to loss of immune system-modulating and/or colonization-blocking species, as well as by stimulating intestinal cells to produce a food source that gives the Salmonella a competitive advantage over other bacteria.90
Social Determinants of Microbiota
Public health researchers have long known of the close relationship between social conditions and inequities and health outcomes. A large body of public health literature documents causal relationships between noncommunicable diseases—such as types 1 and 2 diabetes, cardiovascular disease, colon cancer, breast cancer, and asthma—and socioeconomic status, race, and gender. Other studies have shown how social conditions facilitate the spread and virulence of pathogens, often to the disadvantage of those who are most powerless. More recently, researchers have implicated the loss of microbial diversity and dysbiotic states in many of these diseases. Keisha Findley and her colleagues proposed a mechanistic model involving the immune system for the interaction between social environment, microbiome, and many chronic conditions:
The host immune system is extremely sensitive to changes in the environment and the microbiome. Consequently, perturbations of any kind may result in an aberrant immune response and increased susceptibility to chronic disease. We speculate that a bidirectional interaction exists between the microbiome and psychosocial indicators, and both change in response to the health status of the individual. We recognize that the microbiome may possibly change in response to the immune system, and conversely, the immune system may respond to changes in the microbiome. Furthermore, the same bidirectional relationship observed between the microbiome and psychosocial indicators exists between overall health status and psycho-social indicators.91
In the past few years, scientists have begun exploring the impact of social and economic conditions and the consequences of inequity on the microbiome itself. The relationship should not be surprising, given the impact of factors such as diet, medical practices, or environmental exposures on the microbiota. Tao Ding and Patrick Schloss observed distinct bacterial communities in vaginal and colonic sites in women depending on educational level, a common surrogate for socioeconomic status.92 Ricardo de Mello and associates found greater proportions of Lactobacillus and Bifidobacterium—both associated with beneficial health impacts—in fecal samples of Brazilian children from wealthy backgrounds, compared to children from favelas.93 And they noted the association between these microbes and the Body Mass Index of the children. Another study found a positive correlation between gut biodiversity and neighborhood socioeconomic status.94 A recent study established that the vaginal microbiota of white women as compared with African American women is dominated by Lactobacillus species, which establish a more acidic pH, favorable to vaginal health, a possible consequence of dietary factors.95 African Americans also have much higher rates of colorectal cancer than whites. A study by Goyal and colleagues examined the relationship between dysbiosis and colorectal cancers in African Americans.96 They observed that African Americans with colon cancer show lower levels of butyrate than other racial groups. This compound is a beneficial metabolic product of bacteria associated with high-fiber, low-fat diets. In addition, microbiota have been found to diverge markedly between residents of industrialized and developing nations, urban and rural populations, and between adult and elderly populations.97 Among the latter, it has been shown that gut microbiota is more diverse and healthier among elderly living in communities than in residential facilities.98 To what degree many of these microbial differences respond to socioeconomic conditions or covariates or even genetics, or whether they cause or reflect health conditions has not yet been established.
Capitalism and Micro-Ecological Disturbance
Why would we consider this pattern of disruption of the microbiota and consequent dysbioses to be a manifestation of dynamics intrinsic to the capitalist mode of production and consumption, rather than excesses related to more general tendencies of the “human condition” or more specific and unrelated tendencies of modernity (say, urbanization)? It is worth noting that a burgeoning literature, borne of the looming planetary ecological crises—including climate change, biodiversity loss, introduction of toxic and carcinogenic materials into the biosphere, and disruption of biogeochemical cycling—has increasingly drawn out the connection between these transgressions of planetary ecological boundaries and capitalist production, particularly the inherent tendencies to unending and ever-expanding capital accumulation and its corollary, rampant consumerism. The major environmental influences on the human microbiome all exemplify the tendency of capitalist production and consumption to disrupt ecosystems and attenuate or destroy ecosystem functions and services.
The Food Industry
As mentioned previously, the so-called Western diet has been implicated in a growing number of chronic, noncommunicable diseases (NCDs) associated with modern industrialized societies. In fact, most public health experts express concern about the soaring incidence rates of such conditions as obesity, coronary heart disease, hypertension, stroke, diabetes, certain types of cancer, asthma, chronic hepatic diseases, and chronic renal diseases in developed countries over the past decades. However, these NCDs have now reached epidemic proportions in developing countries as well, with 80 percent of NCD-related deaths now occurring in the lower and middle-income countries, and with two-thirds of global deaths due to NCDs.99
The Western diet is perhaps better characterized as the “industrial diet,” as Anthony Winson calls it in his book of that title, which develops a detailed analysis of the role of the food industry in our nutritional crisis and epidemic of NCDs.100 Winson shows how the proliferation of this unhealthy diet is largely the result of investment and marketing decisions made over the past century by key players in the food industry in the global North, particularly in the United States. These trends have extended to developing countries over the past four decades of neoliberal economics and globalization. As we have shown previously, the microbiome is a crucial mediator between diet and health, with dysbioses implicated in a growing number of these diseases.
The industrial diet is dominated by highly processed, nutritionally stripped and degraded foods, containing excessive amounts of unhealthy fats, refined sugars and simple starch, salt, and various other additives. This diet represents a dramatic departure from the nutritional components that humans consumed during the better part of our history as a species, which shaped our biological evolution and that of our coevolved microbiota. Various lines of research indicate that we are adapted to an omnivorous diet consisting of significant portions of vegetable fiber derived from roots, leaves and shoots, various types of animal protein obtained by foraging, hunting, fishing, or scavenging, and various seeds, nuts, and fruits, as seasonally available. The modern Western diet upends these proportions, adding foodstuffs and nutrients that were scarce or unavailable to our ancestors, while drastically reducing fiber and vitamin-rich fruits and vegetables.101 Nutritionist Loren Cordain and her coauthors note that “although dairy products, cereals, refined sugars, refined vegetable oils, and alcohol make up 72.1 percent of the total daily energy consumed by all people in the United States, these types of foods would have contributed little or none of the energy in the typical preagricultural hominin diet.”102 Furthermore, combinations of those products make up the overwhelming majority of confected, processed foods in the industrial diet.
According to Winson, this diet was largely birthed in the United States in the nineteenth century, when specific conditions of territorial expansion, agriculture, economic development, and processing technology favored the industrialization of food production and processing.103Through the late nineteenth and twentieth centuries, it expanded throughout the global North. Production of refined white flour, made possible with the invention and proliferation of roller-milling, was an early example of this tendency. Mass cultivation of hard spring wheat in the expanding U.S. agricultural frontier was coupled with the new roller-milling and sifting technology to feed a growing market for flour. Contrary to the older stone-milling methods, roller-milling strips the wheat grain of the nutrient and fiber-containing germ and bran, and leaves only the starchy endosperm, which may be further processed through various bleaching methods. The white flour produced in this way can be stored and transported longer and further, but is nutritionally worthless except as a source of calories.104
The transition from free-range, grass-fed beef to feedlot production, another early example, was the result of declining availability of open range lands, the development of feed grain (corn, sorghum, and barley) production, as well as the integration of meat-packing and grain trusts. Feedlot husbandry using increasingly cheap corn allowed the rancher to produce the favored “marbled beef” and to speed up cattle growth from four to five years with grass-feeding to some sixteen months under the feedlot system.105 Turnover time was subsequently shortened further through the use of selective breeding, hormones, and antibiotics. Today, livestock production, sometimes referred to as an Industrial Livestock Operation, is carried out as an enormous factory process, highly monopolized and integrated with other agricultural and processing industries. Corn-fed beef, raised under conditions of inactivity and extreme overcrowding, has a quantitatively and qualitatively different fat content from free-range beef, including far greater overall proportions of fat and skewed proportions of saturated and unsaturated fats, containing distorted proportions of omega-6 and omega-3 fatty acids.106
During the same latter half of the nineteenth century, advances in industrial techniques and transportation allowed producers of refined cane sugar to begin to mass market that product, particularly in England, where consumption rose from some 18 pounds per year per capita in 1840 to 90 pounds by the turn of the century, while the United States followed a similar pattern.107
Further technological advances followed favoring processing, storage, and preservations of produce and livestock products. Industrial food production soon expanded into canned goods, soft-drinks, breakfast cereals, a proliferation of snacks, desserts, and confections, and then the various categories of fabricated, processed, adulterated, and simplified foods that dominate our diets today. Winson explained the profit-driven dynamic of these processed foods:
Generally, more highly processed foodstuffs—goods with more “value added”—have more attractive rates of return for retailers and processors. Foodstuffs that have undergone little or no transformation—for example, table potatoes, fluid milk, eggs, flour, and tomato paste, referred to in the food business as “commodity” products—typically have rather thin profit margins, and indeed some, like fluid milk, are often sold below cost by supermarkets as loss leaders primarily to attract customers to the store. On the other hand, products that have been created out of inexpensive, and often subsidized, raw commodities such as sugar, potatoes, wheat, and corn, with some processing and the addition of inexpensive chemical additives to create “value added,” can be processed into very profitable branded commodities. Their success in the market will depend heavily on expensive advertising, however, and market control.108
Winson characterized processed food commodities bereft of natural nutrients and fiber, and loaded with fat, sweeteners, and salt, as “pseudo foods.”109 He describes three processes that underlie the nutritional degradation of the Western diet: simplification and homogenization of whole food items, such as flour or fruits and vegetables; speedup of turnover time of capital invested in food production, as occurs in livestock production; and production of processed food commodities loaded with “macro-adulterants”—sweeteners, salt, and fats—as well as other additives. Like the adulteration of old, macro-adulteration aims to lower production costs of food commodities. However, these macro-adulterants are also employed to increase consumption of products through appealing appearance, taste, or smell, and by stimulating hard-wired behavioral responses and creating cravings for the food items containing them. And food manufacturers employ these products knowing their detrimental impact on human health.110
The massive expansion of the industrial diet was facilitated by the equally prodigious expansion of mass marketing techniques and product placement by an oligopolistic food industry.111 Branding and name recognition played early and important roles in the expansion of the “industrial diet,” and were key to the success of such well-known early products as Kellogg’s corn flakes and Coca-Cola soft drink. In 2006, alone, the nine top processed food vendors invested over $9 billion in advertising in the United States, the vast majority of which promoted pseudo-foods.112
In the latter part of the twentieth century, supermarkets and fast-food chains, together with chain restaurant establishments and convenience stores, emerged and grew explosively to become the primary purveyors of the industrial diet. The top ten U.S. supermarkets, controlling 80 percent of supermarket grocery sales, realized over $400 billion in sales in 2006. In a survey of shelf space in supermarkets, Winson found that
The average linear footage devoted to pseudo foods ranged from 26 to 37 percent of the total of linear footage devoted to edible goods in the stores we surveyed. For the twelve stores sampled in our study, the average proportion of pseudo foods of all foods measured was 31 percent. Pseudo foods are more likely to be found on the shelves that constitute the central area of each store, where they range from 35 to 44 percent of all edible products. This, of course, is the part of most supermarket food environments where entire aisles are devoted to bulk candies and chocolates, to cookie displays, and to soft drinks and high-fat and high-sodium potato- and corn chip products.113
In his analysis, Winson calculated that some 70 percent of shelf space in convenience stores is dedicated to pseudo foods.114
Turning to fast-food chains, the same author cited a study that noted that their menu offerings “typically contain approximately 1,100 calories per 100 grams, whereas the average British diet is estimated to contain 670 calories per 100 grams. The caloric load of the fast-food meal, moreover, is noted to be twice the energy density of a healthy diet (considered to be 525 calories per 100 grams).”115 Another study cited assessed the excessive amounts of salt, trans and total fats, and sugar in popular fast-food combo meals.116
During the last quarter of the twentieth century, prompted by tightening markets in the developed countries and lured by cheap labor and land in developing markets in the global South, the global food giants began outsourcing production, and marketing their products on a massive scale to the developing world, facilitated by neoliberal financial policies and trade agreements. Consequently, foreign direct investment (FDI) by major food corporations in the global South has rapidly expanded. In particular,
Initial entry into markets focuses on packaged and highly processed foods that are marketed as exotic, convenient, and modern. Such investment has become so successful that food processing now has the highest amount of FDI compared to other parts of the food system. Most astonishing is the fact that FDI in the global processed foods market is more important than FDI in global trade. This fact is extremely important because it reiterates just how much market power is involved within the global food industry—particularly the sector that markets the most unhealthy, nutrient-poor food. Such extensive investment by transnational Big Food companies has created food systems that are increasingly influenced by external forces, rather than forces within the domestic country.117
FDI in food production and sales in developing countries has increased access to and promotion of unhealthy processed foods, fostered the spread of global supermarket, fast-food, and restaurant chains, facilitated penetration of the market and displacement of local food items by pseudo-foods, and increased control over local food systems by transnational corporations.118
Consequently, FDI has favored the substitution of nutrient-rich local produce and diets with industrial diets poor in nutrients and rich in fat, sugar, and salt. In addition to affecting consumers, FDI has led to severe impacts on local producers who cannot compete with the technological advantages and economies of scale of large corporations, and who are thus displaced from agricultural or food preparation activities, and driven into rural or urban poverty. As Winson explained, “The long-standing unity of production and consumption characterizing peasant production in most parts of the world for millennia is being broken today on a phenomenal scale.”119 The overall effect has been to adversely impact nutritional status and give rise to the duality of rising chronic metabolic disorders side-by-side with starvation, both symptoms of malnutrition.
Various writers discuss the impact of urbanization on the adoption of the Western diet. Urbanization is “not, of course, some natural process but is itself in large part the product of the expropriation of masses of rural smallholders in country after country.”120 More than 54 percent of the global population currently lives in cities, and this is expected to grow to 66 percent by 2050, with the bulk of this growth occurring in Asia and Africa.121 Urban expansion paves the way for dietary change, in conjunction with other aspects of the neoliberal program, in a number of ways. The rural-urban migration deprives migrants of access to agricultural production, as does the increase in lands occupied by big investors. It throws masses of people—and increasingly, women—into the low-wage urban labor force (or unemployment), thus imposing both financial and time constraints on household food preparation. It brings these masses into contact with cheap processed foods, and particularly, fast- and street-foods, and immerses them in an increasingly market-driven culture favoring these items.122 For example, in Tanzania, low-middle-income groups derive 70 percent of their caloric intake from street foods.123
Winson elaborates on the ways these changes paved the way for supermarket and fast-food chain expansion into developing country markets:
Recent research has documented the unprecedented pace by which the supermarket form of retail food selling is transforming Latin America, Asia, and Africa. A series of changes in the structures of economies in these regions have opened up new opportunities for the supermarket retail form. Among the most important of these changes are rapid urbanization; expansion of the middle class and with it a rise in disposable incomes for this segment of the population and the ability to purchase refrigerators; significant increases in female labor force participation; and the rapid growth of car culture and access to public transport.124
While such expansion is uneven in the global South, in Latin America both supermarkets and convenience stores have expanded as much in ten years as they have in five decades in the United States, to the point where supermarkets control up to 80 percent of retail food sales in Brazil and close to 60 percent in Argentina, Mexico, and Panama. While local entrepreneurs may have launched the first supermarkets, this sector is increasingly dominated by transnational chains, with some 70 to 80 percent of Latin American supermarket chains in the hands of the top five global firms.125
In the developed countries, supermarkets have responded, to some degree, to increasing public nutritional awareness and healthy food movements, with a greater diversity of healthier food items, at least for certain social classes. But in the developing world, “supermarkets have another role here from a nutritional standpoint: introducing large numbers of people among the newly emergent middle classes to ready-to-eat breakfast cereals, processed cake mixes, reconstituted and artificially sweetened fruit juices, industrial baked goods, processed meats, and other goods of the industrial food system with which they may have only passing familiarity.”126
Similarly, fast-food chains have rapidly spread into the expanding urban markets in the global South. By 2008, McDonald’s, the largest global fast-food chain, “could boast that it had a thousand restaurants in China alone, and over thirty thousand restaurants worldwide.”127 Of the Yum! Brands megafirm, which includes KFC, Pizza Hut, and Taco Bell, Winson writes:
Worldwide sales for this transnational were in the $30 billion range in 2007. This rival firm has itself a strong global presence, with restaurants in over a hundred countries by 2005. Indeed, it opened 780 restaurants in that year alone, boasting a total of an astounding 34,000 restaurants around the globe by 2005, outnumbering McDonald’s in number of restaurant units…. Yum! Brands is especially strong in rapidly colonizing the world’s fastest growing markets in the global South, with China being its priority target…. Yum! Brands reported 22 percent annual growth in its China business in 2005, along with franchise business sales growing 10 percent in the Caribbean and Latin America, 17 percent in the Middle East and North Africa, and 20 percent in South Africa.128
A massive public health, nutritionist, and food justice literature confirms that in both developed and developing nations, class and other social relations between dominant and subaltern groups determine diet and nutrition.129 Numerous studies have also documented the relationship between socioeconomic status, access to nutritional foods, and chronic metabolic disease states, in addition to the classical diseases of malnutrition, although some controversies rage over the modalities through which forms of oppression play out in diet and NCDs.130 And it is increasingly apparent that disruption of our microbial ecosystems via the normal functioning of capitalist production and marketing is a critical link in these relationships, just as it has shown itself to be in macro realms. Moreover, the micro- and macro-ecological domains are inseparably interconnected, as Rob Wallace shows in his book Big Farms Make Big Flu.131
Big Pharma
There are two major pathways through which antibiotics gain access to our microbiota. First, there is the rampant use of antibiotics in health care. The second is the even more profligate use of antibiotics as growth stimulants and prophylactics in the livestock industry. While the latter use is of great importance for the proliferation of antibiotic resistance in bacteria, the former has a greater known impact on the human microbiota, and so I will focus on human antibiotic use. However, it is worth noting that, globally, twice the amount of antibiotics are used for livestock as in human health applications.132 Antibiotic residues have been found in animal products for human consumption, including meat, milk, farmed and wild fish, and honey, in many cases above allowable limits, and these have the potential to disrupt human microbiota, as has been shown in studies of subtherapeutic doses.133
The pharmaceutical sector is the world’s most profitable, alongside banking. The ten largest pharmaceutical corporations made a combined profit of $90 billion in 2013, for a net profit of 19 percent.134 In 2009, global antibiotic sales were worth $42 billion, equivalent to 5 percent of the pharmaceutical market.135 This figure rose to $43.55 billion in 2012, and is expected to grow to $45.09 billion by 2019.136 And, although antibiotics are cheaper than other pharmaceuticals, a report by the Center for Disease Dynamics, Economics and Policy observes that “antibiotics are still very profitable. In 2004, they were the third highest earning drug class behind central nervous system and cardiovascular drugs, bringing in $26 billion to $45 billion per year…. Despite shorter courses, many more people take antibiotics than they do other types of drug, and antibiotics can even become ‘blockbusters.'”137
However, while antibiotic sales have continued to increase, the major drug companies have halted research and development on new classes of antibiotics needed to combat emergent antibiotic resistant bacteria, citing low returns on investments and tight regulatory requirements for bringing antibiotics to the market.138
As old patents lapsed, the major drug firms outsourced or contracted much of antibiotic production to generic manufacturers in countries with relatively low sale prices and low costs of production for existing antibiotics, particularly China and India.139 As one indicator, by 2010, generic antibiotics represented over 80 percent of global prescriptions.140 India currently hosts a major part of the world’s production of bulk drugs, while China produces the major share of active pharmaceutical ingredients used in global antibiotic manufacture, supplying much of India’s bulk drug production.141 Major health care and pharmaceutical corporations and pharmacy chains then work up or simply market the final products.142 Discussing the shift to generic antibiotic use in both human and veterinary medicine, Pierre-Louis Toutain and Alain Bosquet-Melou noted that, “competition between generics and also between generics and branded antibiotics (usually forced to lower their prices in order to remain competitive against the cheaper generic versions) leads to more aggressive promotion for the use of antibiotics both in human and veterinary medicine.”143 In turn, according to these authors, the inundation of these markets with cheap generic antimicrobials has led to increased consumption.
Today, antimicrobials are the most frequently prescribed drugs in the pharmaceutical arsenal. Per capita human consumption of antibiotics remains highest in industrialized countries. India, China, and the United States were the largest overall consumers in 2010, with total use at 12.9 x 109, 10 x 109, and 6.8 x 109 standard units, respectively.144 Global antibiotic consumption increased by an estimated 36 percent between 2000 and 2010, to over 63,000 tons.145Approximately three-quarters of the increase in global consumption was in the BRICS countries of Brazil, Russia, India, China, and South Africa.146 In the United States alone, antibiotics were prescribed at a rate of 842 courses per 1,000 people in 2011, for a total of 262 million courses.147 However, although global antibiotic use is increasing, it should be noted that there is a global disparity in antibiotic consumption, with much of the population of the global South denied access to necessary antibiotics, where “no access and delays in access to antibiotics kill more people than antibiotic resistance.”148
According to the Center for Disease Dynamics, Economics and Policy report, “from 20 to 50 percent of total [human] antibiotic use is estimated to be inappropriate,” which is defined as “the use of antibiotics when no health benefit is possible” and “the suboptimal use of antibiotics for responsive conditions.”149 The report noted that in U.S. hospitals surveyed, “broad-spectrum antimicrobial therapy was commonly prescribed to inpatients even when clinical signs of infection were not present, and this treatment was not de-escalated or discontinued even when cultures did not show evidence of bacterial infection.”150
What has led to the massive overuse of antibiotics that is driving both the scourge of antibiotic resistance and disruptions of the human microbiota? Over-prescription and irrational consumption are aspects of the market-driven health care model that dominates in almost all parts of the globe. Under the prevailing form of health care, most countries have come to place a heavy focus on clinical medicine, and particularly secondary and tertiary care, rather than upstream prevention, that is, by addressing aspects such as the environmental and social determinants of health. “Taken together, the evidence indicates that prescribing medicines has become a dominant, if not the dominant, form of health care in western societies and its role in middle-income countries is growing rapidly,” writes medical sociologist Joan Busfield.151
Our market-based health care model has long been dominated by the pharmaceutical industry. According to Busfield, direct marketing and promotion of their products represent important mechanisms employed by the pharmaceutical industry to drive that market.152 In the major industrialized nations, marketing expenditures represent roughly twice the amount as research and development expenditures.153 Medical sociologist John Abraham observed that, in the 10 years prior to 2005, British pharmaceutical companies cut research personnel by 2 percent, while marketing staff grew by 59 percent.154
Through promotional activities directed at consumers and providers, the pharmaceutical industry has encouraged consumers to expect pharmacological answers to health problems and to demand medications from providers.155 Further, according to Abraham, pharmaceutical companies encourage “collaborative” or “active” consumerism, including through funding for patient organizations.156 In addition, he notes that “consumerism has an ideological dimension, namely the discursive appropriation of the health needs of patients as the demands of consumers in a market…such discourse is distinct from patients’ actions and needs, and may not even be derived from them.”157 He further observed that “the ‘expert patient’ discourse needs to be put in the context of the interests of those planning to provide the ‘information’ intended to construct ‘patient expertise,’ namely a profit-seeking industry with a record of promoting its products with misleading information to doctors.”158
For their part, physicians are targeted by promotional literature through the mail, in journals, and via other venues. They receive visits by business representatives and are invited to industry-sponsored conferences. Various studies indicate that these promotional efforts pay off in recommendations and prescriptions by physicians.159 Physicians are funded to participate in product development or invited to promote specific products at symposia.160Medical practice, together with patient demands, facilitates excessive pharmaceutical dissemination, as physicians are prompted to prescribe medications in order to show efficacy even in absence of need.161 In addition, in a number of countries, including China and India (where prescriptions are not required), drug companies offer financial incentives to doctors to push their products, particularly antibiotics.162
The processes known as “medicalization” or “pharmaceuticalization” are deeply imbricated in our medical model.163 The terms signify slightly different aspects of the social construction and delimitation of what constitute medical issues, which then become amenable to the proper medication, or even the extension of drug therapy outside of the domain of clinical medicine.164 According to Busfield, the drug companies are the “active drivers” in this process.165 Contrary to the pharmaceutical industry’s portrayal of its efforts “to support medicine’s therapeutic endeavors,” Busfield stated, “the evidence indicates that the industry plays an active role in shaping those endeavors.”166
Medicalization received its initial impetus as a result of the postwar expansion of consumerism. Elizabeth Siegel Watkins observes that “aspects of postwar culture fostered an appetite for prescription drugs: specifically, a fascination with technological solutions.”167 As she explains, “consumers eagerly adopted new drugs in much the same way that they adopted TV dinners and cake mixes.” In the postwar years, industry, government, and the media pointed to Alexander Fleming’s discovery of penicillin and Jonas Salk’s polio vaccine as heralding final victory in the war on infectious disease.168 The pharmaceutical industry then proceeded to pump out antibiotics, proclaiming their low cost and safety. All of this was in spite of the warning Fleming issued about the danger of antibiotic resistance at his Nobel Prize award ceremony in 1945.
The processes of pharmaceuticalization and medicalization gained further momentum with the deregulation, commodification, and privatization of the neoliberal era. According to Jill Fisher, “neoliberalism extends the commodification of health in new ways; under its governing logic, consumption is not only a right but also an obligation if one wants health care at all.”169She noted that
Patients as consumers have embraced the neoliberal logics of health care so that they too see illness in reductionist terms and seek pharmaceuticals as targeted magic bullets. This orientation toward health and medicine has been referred to as the pharmaceuticalization of health care, in which the conditions of health and illness are ever more cast in terms of products that can be purchased by health-engaged consumers. A medical system that revolves around pharmaceuticals contributes to a culture of medical neoliberalism. It ties together the commodification of health care with the fragmentation of the body where illness is treated in terms of discrete systems for which there are tailored products.170
In the United States, European Union, and United Kingdom, government regulatory agencies have favored the interests of the pharmaceutical industry and facilitated market development and pharmaceuticalization, despite their ostensible mandate to regulate the industry on behalf of public health. Simon J. Williams and colleagues cited various studies showing “corporate bias and privileged access” of the pharmaceutical industry to the U.S. Food and Drug Administration and its British counterpart, the Medicine and Health Care Products Regulatory Agency.171 The results include deregulation of pharmaceuticals, relaxation of safety standards and review requirements, and reduction of review times on patentable drugs.172 In addition, Western regulatory agencies have undertaken joint initiatives, such as the International Conference on Harmonisation, which seek to standardize regulatory frameworks to accommodate development of markets and outsourcing of research and development and production to developing countries.173
Of particular relevance to the overuse of antibiotics, Abraham described the drivers and significance of pharmaceuticalization:
increased pharmaceuticalization is not fuelled primarily by growth in pharmaceutical provision to meet, and advance, health needs. Rather the sociological factors of consumerism, deregulatory state policies, industry’s commercial priorities and product promotion, and medicalization have been expanding pharmaceuticalization in ways that are largely outside such provision. It may be that marketing does not necessarily create false needs…but it may create false claims and expectations about the capacity of pharmaceuticals to meet those needs. Moreover, the ideological appropriation of patients’ needs as consumer preferences in a market means that public health requirements, which are poorly expressed in marketing processes such as antibiotic development and protection from drug injury, are inappropriately neglected by an industry supposed to advance health.174
Medicalization and pharmaceuticalization have directly and indirectly favored the excessive and irrational use of antibiotics. The use of antibiotics as growth stimulants in animal feed, or their prescription for viral diseases or even as placebos, represent clear instances of pharmaceuticalization. Furthermore, these processes have forged a social-psychological framework that encourages profligate consumption of antibiotics. Within that framework, the industry’s expanded and outsourced production of cheap and easily accessible generics, aggressive marketing to both consumers and providers, and control over pharmaceutical research and its dissemination have driven antibiotic overuse and wasteful consumption.
Our current medical model relies on the much-touted “miracles of modern medicine,” on magic-bullet cures for diseases. In this sense, capitalist medicine follows the pattern evident in capitalist agriculture, capitalist energy production, and indeed, the capitalist mode of production in general, of disaggregating complex ecosystems to tease out marketable, profitable commodities, and then offering magic-bullet solutions to the environmental problems such production engenders. Infectious diseases are not merely products of pathogens but of social and ecological disturbance, including those at the level of microbial ecosystems. Our form of economic development has disrupted these ecosystems at both macro and micro levels. Antibiotics are necessary, but cannot substitute for a more ecologically integral approach to human health. In turn, such magic bullets, themselves, are disconnected from ecological or biological contexts and offered without integral consideration of consequences, producing further disruptions, for which new magic bullets are devised.
The proliferation of antibiotic-resistant bacteria and the now desperate search for new antibiotics, or the epidemic of potentially dysbiosis-induced noncommunicable diseases and the booming literature on pre- and probiotics to address them, are both further expressions of the failure of the current medical paradigm.
This reductionist model is expressed as “war on pathogens.” This war, with its exclusive focus on “bad microbes” and therapeutic agents aimed narrowly at exterminating them, was initiated by Louis Pasteur, Robert Koch, and others at the turn of the century. It pushed aside the equally robust microbial ecosystem narratives traced out by biologists such as Theodor Escherich, Arthur Isaac Kendall, and Elie Metchnikoff. Kendall offered the view that the gut was the “perfect incubator” for innumerable mutualistic bacteria, some of which might even defend their hosts against pathogens. Even Pasteur believed that many gut bacteria were beneficial.175
Conclusion
The antibiotic resistance crisis and the Western diet problem have been on the public health radar for some time. But the potential pharmaceutical and industrial food effects on the microbiome have received little attention. While a few authors have addressed the public health implications of microbiome research and dysbiosis, they have not been taken up in any systematic way.176 Nevertheless, there are far-reaching conceptual and practical implications of these phenomena for human health and ecology.
For the most part, the microbiome as a health-related phenomenon has been approached within the framework of the prevailing pharmaceutical industry-driven medical model, in yet another example of medicalization. Almost every journal article dealing with microbiota and dysbiosis notes the potential for the pharmaceutical industry to develop probiotics or prebiotics, or standardized microbial assemblages for transplant, or genetically modified symbionts to enhance gut function or block pathogens, or other marketable therapies derived from deeper knowledge of the microbiome.177
All of these therapies, in themselves, are of potential benefit to human health. However, if history is any guide, in the hands of the for-profit pharmaceutical industry, the market will guide their development and production and their full benefits will either be economically inaccessible to the majority of our populations, or they will fail to garner the investment interest of the major research firms. However, this approach fails to address the underlying reasons for dysbiosis. To address those causes requires major social and economic shifts, which, if climate change is any indication, are not achievable within our current social order.
In the first place, dysbiosis must be dealt with ecologically, recognizing that our own bodies are ecosystems, integrated at ever larger scales with our biosphere. Concretely, this means that our “ecosystem functions and services”—principally our health—depend on specific qualitative and quantitative states of biodiversity; that is types, functions and numbers of, and interrelations between, microbiota. Altered environmental factors—social and economic—can tip these states into dysfunctionality.
Our food is the major environmental influence on microbiota health. Under the impetus of the market, diet has radically changed in industrialized nations and is rapidly changing in industrializing nations. Instead of the ancestral diets that our species and our microbial communities coevolved to assimilate, we now consume highly processed diets bereft of sufficient fiber and complex plant carbohydrates, and overwhelmingly rich in fats, salt, and simple sugars. These changes have favored alteration or disruption of the microbiota that coevolved as mediators for a host of metabolic and physiological functions. These alterations and disruptions do not represent “adaptations” to new dietary regimes, but rather literal metabolic rifts with negative consequences for our health. Thus, a radical reorganization of our food production, supply, and promotion, as well as our nutritional education, is in order.
Neither our dominant agricultural system nor the food industry is geared toward producing an appropriate balance of diverse and nutritional items that are affordable to all. Agriculture focuses primarily on producing competitively marketable, profitable commodities for the food processing industry and the consumer, with a concomitant loss of diversity and nutritional value. Beyond producing commodities that fail to fulfill nutritional needs, our current large-scale capitalist agriculture is ecologically unsustainable and relies on inputs that are also destructive of human and ecosystem health. Therefore, production decisions should not be left in the hands of agribusinesses, but should be socialized and placed in the hands of councils of associated farmers, agricultural workers, and the general public. Production itself should be assumed by small farmers, worker cooperatives, or publicly owned farms, according to crops, geography, local tradition, and needed economies of scale. Production of agricultural inputs, as well—such as fertilizers and pesticides—should be taken out of the hands of the agrochemical conglomerates and placed under the control of accountable public entities. Their use can be minimized and in many cases eliminated if farming is approached ecologically, to improve field and soil habitat that promotes healthy soils, the presence of beneficial organisms, leading to healthy plants and animals.
The food industry has geared its production to dysbiosis-inducing, food commodities, larded with addictive salts, fats, and sugars. Class and race play a role in the investment decisions of the food industry, whereby nutritionally poor foods, whose detrimental impact is mediated by the microbiota, are disproportionately marketed to low-income and marginalized populations. Meanwhile, better-off groups, while still subject to unhealthy market items, have access to a greater variety of healthy dietary choices. A healthy diet must be seen as a human right, and dietary recommendations must begin to take into account impact on the microbiome. Food processing and distribution must be under the control of the public (community) while food production decisions are made by associated production workers using ecological principles, in accordance with nutritional frameworks that provide for our integral needs.
As for the pharmaceutical industry, we have presently reached the absurd contradiction in which mass production of antibiotics by the drug corporations, together with the consumerism they engendered, has produced a crisis of antibiotic resistant bacteria and disruption of human and other microbial ecosystems. Yet, citing low rates of profit, they refuse to develop new antibiotics that can cope with the onslaught of multiple resistant bacterial strains. Industry proposals to undertake research represent little more than efforts to extort relaxation of safety and testing regulations and subsidies from taxpayers.178 In contrast, the pharmaceutical and health product giants continue to reap profits through outsourced production of present generation antibiotics in generic or branded form. As long as a profit is to be made, they will continue to expand production and drive a market based largely on excessive and irrational antibiotic use. Together with the obscene costs of many vital pharmaceuticals, this bespeaks the need to socialize the pharmaceutical industry and subject it to a national plan to produce necessary medications at prices accessible to all, by placing it under the democratic control of its workforce, health professionals and consumers, and by subjecting its research and ledgers to public scrutiny.
As amply shown in the foregoing discussion, the human microbiota is a critical mediator between social determinants and physiological states and health outcomes. Access to adequate nutrition, income, education, health services, and reliable sanitary infrastructure, as well as exposure to environmental hazards, reflecting existing social power relations, all shape the microbiota. These power relations—social class, race, and gender—loom in the background as upstream environmental modulators of dysbiotic states. Insofar as the field of public health has long recognized that oppression and exploitation are causal to health disparity and poor health outcomes, and strives for their elimination, the human microbiome provides further compelling evidence of negative health impacts and motivation to struggle to abolish racism and sexism, and the exploitative relationship between capital and the majority of our populations.
Social, economic, and health inequity, like the ability of capital to profit at public expense, rely on the power of the state, whether through tax policy, laws and regulatory regimes, financial subsidies and incentives, or trade policy. Recent studies provide additional evidence in support of an increasingly widespread public perception of corporate domination of government, and the latter’s divorce from public needs. It is reasonable to ask how economic and social policy might be structured by criteria of human health, life quality, and ecological sustainability, instead of market share and profitability. How might society as a whole democratically decide and plan how to invest its productive resources to best serve those needs? What types of public control are needed to assure that regulatory agencies are free of corporate interests, accountable and transparent? And how might research and development of drugs, foods, and other necessary goods and services also be removed from corporate control and rendered subject to public scrutiny? How might our institutions be changed or what kinds of institutions must be forged to pursue the elimination of power differentials in society, particularly those inhering to oppressive relationships between groups, and exploitation of the majority by a minority, all of which produce adverse health outcomes and ecological disruption?
Notes
- ↩ John Bellamy Foster, “Marx’s Theory of Metabolic Rift: Classical Foundations for Environmental Sociology,” American Journal of Sociology 105, no. 2 (1999): 366–405.
- ↩ Brett Clark and Richard York, “Carbon Metabolism: Global Capitalism, Climate Change, and the Biospheric Rift,” Theory and Society 34, no. 4 (2005): 391–428; Rebecca Clausen and Brett Clark, “The Metabolic Rift and Marine Ecology: An Analysis of the Ocean Crisis within Capitalist Production,” Organization & Environment 18, no. 4 (2005): 422–44.
- ↩ Peter J. Turnbaugh et al., “The Human Microbiome Project: Exploring the Microbial Part of Ourselves in a Changing World,” Nature 449 no. 7164 (2007): 804.
- ↩ Courtney J. Robinson, Brendan J. M. Bohannan, and Vincent B. Young, “From Structure to Function: The Ecology of Host-Associated Microbial Communities,” Microbiology and Molecular Biology Reviews 74, no. 3 (2010): 453–76; Turnbaugh et al., “The Human Microbiome Project.”
- ↩ Trisha Gura, “Nature’s First Functional Food,” Science 345 no. 6198 (2014): 747–49; Andrew H. Moeller, “Cospeciation of Gut Microbiota with Hominids,” Science 353, no. 6297 (2016): 380–82.
- ↩ Gura, “Nature’s First Functional Food.”
- ↩ Gura, “Nature’s First Functional Food”; Ed Yong, I Contain Multitudes: The Microbes Within Us and a Grander View of Life (New York: Random House, 2016).
- ↩ Ron Sender, Shai Fuchs, and Ron Milo, “Are We Really Vastly Outnumbered? Revisiting the Ratio of Bacterial to Host Cells in Humans,” Cell 164, no. 3 (2016): 337–40.
- ↩ Xing Yang et al., “More than 9,000,000 Unique Genes in Human Gut Bacterial Community: Estimating Gene Numbers Inside a Human Body,” PLoS One 4, no. 6 (2009): e6074.
- ↩ Yong, I Contain Multitudes.
- ↩ Ainslie E. F. Little et al., “Rules of Engagement: Interspecies Interactions that Regulate Microbial Communities,” Annual Review of Microbiology 62 (2008): 375–401.
- ↩ Yong, I Contain Multitudes.
- ↩ Scott F. Gilbert, Jan Sapp, and Alfred I. Tauber, “A Symbiotic View of Life: We Have Never Been Individuals,” Quarterly Review of Biology 87, no. 4 (2012): 325–41; Yong, I Contain Multitudes.
- ↩ Eva Boon et al., “Interactions in the Microbiome: Communities of Organisms and Communities of Genes,” FEMS Microbiology Reviews 38, no. 1 (2014): 90–118; Sascha Krause et al., “Trait-Based Approaches for Understanding Microbial Biodiversity and Ecosystem Functioning,” Frontiers in Microbiology 5, no. 251 (2014): 1–10; Robinson, Bohannan, and Young, “From Structure to Function.”
- ↩ Catherine A. Lozupone et al., “Diversity, Stability and Resilience of the Human Gut Microbiota,” Nature 489, no. 7415 (2012): 220–30.
- ↩ Les Dethlefsen and David A. Relman, “Incomplete Recovery and Individualized Responses of the Human Distal Gut Microbiota to Repeated Antibiotic Perturbation,” Proceedings of the National Academy of Sciences 108, Supplement 1 (2011): 4554–61; Robert T. Paine, Mia J. Tegner, and Edward A. Johnson, “Compounded Perturbations Yield Ecological Surprises,” Ecosystems 1, no. 6 (1998): 535–45.
- ↩ Amy Langdon, Nathan Crook, and Gautam Dantas, “The Effects of Antibiotics on the Microbiome throughout Development and Alternative Approaches for Therapeutic Modulation,” Genome Medicine 8, no. 1 (2016): 39.
- ↩ Mark R. Charbonneau et al., “A Microbial Perspective of Human Developmental Biology,” Nature 535, no. 7610 (2015): 48–55.
- ↩ Maria Carmen Collado et al., “Human Gut Colonization May Be Initiated in Utero by Distinct Microbial Communities in the Placenta and Amniotic Fluid,” Scientific Reports 6, no. 23129 (2016).
- ↩ Samuli Rautava et al., “Microbial Contact during Pregnancy, Intestinal Colonization and Human Disease,” Nature Reviews Gastroenterology and Hepatology 9, no. 10 (2012): 565–76; Juan Miguel Rodríguez et al., “The Composition of the Gut Microbiota throughout Life, with an Emphasis on Early Life,” Microbial Ecology in Health and Disease 26, no. 1 (2015): 26050.
- ↩ Charbonneau et al., “A Microbial Perspective of Human Developmental Biology”; Gura, “Nature’s First Functional Food.”
- ↩ Yuliya E. Borre et al., “Microbiota and Neurodevelopmental Windows: Implications for Brain Disorders,” Trends in Molecular Medicine 20, no. 9 (2014): 509–18; Thomas Gensollen et al., “How Colonization by Microbiota in Early Life Shapes the Immune System,” Science 352, no. 6285 (2016): 539–44; Rodríguez et al., “The Composition of the Gut Microbiota throughout Life.”
- ↩ Lozupone et al., “Diversity, Stability and Resilience of the Human Gut Microbiota”; Moya, A., &Ferrer, M. 2016. Functional redundancy-induced stability of gut microbiota subjected to disturbance. Trends in microbiology, 24(5), 402-413.
- ↩ Andrés Moya and Manuel Ferrer, “Functional Redundancy-Induced Stability of Gut Microbiota Subjected to Disturbance,” Trends in Microbiology 24, no. 5 (2016): 402–13.
- ↩ Nicola Segata, “Gut Microbiome: Westernization and the Disappearance of Intestinal Diversity,” Current Biology 25, no. 14 (2015): R611–13; Erica D. Sonnenburg et al., “Diet-Induced Extinctions in the Gut Microbiota Compound Over Generations,” Nature 529, no. 7585 (2016): 212–15.
- ↩ Stephen M. Collins, Michael Surette, and Premysl Bercik, “The Interplay between the Intestinal Microbiota and the Brain,” Nature Reviews Microbiology 10, no. 11 (2012): 735–42; Felix Sommer and Fredrik Bäckhed, “The Gut Microbiota—Masters of Host Development and Physiology,” Nature Reviews Microbiology 11, no. 4 (2013): 227–38.
- ↩ Kenya Honda and Dan R. Littman, “The Microbiota in Adaptive Immune Homeostasis and Disease,” Nature 535, no. 7610 (2016): 75–84; Yun Kyung Lee and Sarkis K. Mazmanian, “Has the Microbiota Played a Critical Role in the Evolution of the Adaptive Immune system?” Science 330, no. 6012 (2010): 1768–73; Christoph A. Thaiss et al., “The Microbiome and Innate Immunity,” Nature 535, no. 7610 (2016): 65–74.
- ↩ Honda and Littman, “The Microbiota in Adaptive Immune Homeostasis and Disease.”
- ↩ Thomas Gensollen et al., “How Colonization by Microbiota in Early Life Shapes the Immune System”; Pajau Vangay et al., “Antibiotics, Pediatric Dysbiosis, and Disease,” Cell Host & Microbe 17, no. 5 (2015): 553–64.
- ↩ Andreas J. Bäumler and Vanessa Sperandio, “Interactions between the Microbiota and Pathogenic Bacteria in the Gut,” Nature 535, no. 7610 (2016): 85–93; José E. Belizário and Mauro Napolitano, “Human Microbiomes and Their Roles in Dysbiosis, Common Diseases, and Novel Therapeutic Approaches,” Frontiers in Microbiology 6, no. 1050 (2015); Michel Fons, Ana Gomez, and Tuomo Karjalainen, “Mechanisms of Colonisation and Colonisation Resistance of the Digestive Tract Part 2: Bacteria/Bacteria Interactions,” Microbial Ecology in Health and Disease 12, no. 2 (2000): 240–46; Ansel Hsiao et al., “Members of the Human Gut Microbiota Involved in Recovery from Vibrio CholeraeInfection,” Nature 515, no. 7527 (2014): 423–26; Valerio Iebba et al., “Eubiosis and Dysbiosis: The Two Sides of the Microbiota,” New Microbiology 39, no. 1 (2016): 1–12; R. Elizabeth Sockett and Carey Lambert, “Bdellovibrio as Therapeutic Agents: A Predatory Renaissance?” Nature Reviews Microbiology 2, no. 8 (2004): 669–75.
- ↩ Sommer and Bäckhed, “The Gut Microbiota.”
- ↩ Sommer and Bäckhed, “The Gut Microbiota.”
- ↩ Collins, Surette, and Bercik, “The Interplay between the Intestinal Microbiota and the Brain.”
- ↩ Collins, Surette, and Bercik, “The Interplay between the Intestinal Microbiota and the Brain.”
- ↩ Collins, Surette, and Bercik, “The Interplay between the Intestinal Microbiota and the Brain”; Jane A. Foster and Karen-Anne McVey Neufeld, “Gut–Brain Axis: How the Microbiome Influences Anxiety and Depression,” Trends in Neurosciences 36, no. 5 (2013): 305–12.
- ↩ Collins, Surette, and Bercik, “The Interplay between the Intestinal Microbiota and the Brain.”
- ↩ Yan Wang and Lloyd H. Kasper, “The Role of Microbiome in Central Nervous System Disorders,” Brain, Behavior, and Immunity 38 (2014): 1–12.
- ↩ Wang and Kasper, “The Role of Microbiome in Central Nervous System Disorders.”
- ↩ Collins, Surette, and Bercik, “The Interplay between the Intestinal Microbiota and the Brain”; Wang and Kasper, “The Role of Microbiome in Central Nervous System Disorders”; Foster and Neufeld, “Gut–Brain Axis.”
- ↩ Kristina B. Martinez, Vanessa Leone, and Eugene Chang, “Western Diets, Gut Dysbiosis, and Metabolic Diseases: Are They Linked?” Gut Microbes 8, no. 2 (2017):130–42.
- ↩ Paine, Tegner, and Johnson, “Compounded Perturbations Yield Ecological Surprises.”
- ↩ David U. Hooper, “Effects of Biodiversity on Ecosystem Functioning: A Consensus of Current Knowledge,” Ecological Monographs 75, no. 1 (2005): 3–35; David Tilman, Forest Isbell, and Jane M. Cowles, “Biodiversity and Ecosystem Functioning,” Annual Review of Ecology, Evolution, and Systematics 45 (2014): 471–93.
- ↩ Debra L. Wohl, Satyam Arora, and Jessica R. Gladstone, “Functional Redundancy Supports Biodiversity and Ecosystem Function in a Closed and Constant Environment,” Ecology 85, no. 6 (20014): 1534–40.
- ↩ Robert A. Britton and Vincent B. Young, “Interaction between the Intestinal Microbiota and Host in Clostridium Difficile Colonization Resistance,” Trends in Microbiology 20, no. 7 (2012) 313–19; Les Dethlefsen and David A. Relman, “Incomplete Recovery and Individualized Responses of the Human Distal Gut Microbiota to Repeated Antibiotic Perturbation,” Proceedings of the National Academy of Sciences 10, Supplement 1, (2011): 4554–61.
- ↩ Asu Erden, “The Very Microbes that Helped Us Evolve Now Make Us Sick,” Aeon, February 14, 2017, http://aeon.co; Seth Rakoff-Nahoum and Ruslan Medzhitov, “Role of the Innate Immune System and Host-Commensal Mutualism,” in Tasuku Honjo and Fritz Melchers, eds., Gut-Associated Lymphoid Tissues(Berlin: Springer, 2006), 1–18; Graham A. Rook, “Regulation of the Immune System by Biodiversity from the Natural Environment: An Ecosystem Service Essential to Health,” Proceedings of the National Academy of Sciences 110, no. 46 (2013): 18360–67.
- ↩ Stig Bengmark, “Gut Microbiota, Immune Development and Function,” Pharmacological Research 1, no. 69 (2013): 87–113; Martinez, Leone, and Chang, “Western Diets, Gut Dysbiosis, and Metabolic Diseases”; Graham A. W. Rook, Charles L. Raison, and Alan Lowry, “Microbial ‘Old Friends,’ Immunoregulation and Socioeconomic Status,” Clinical & Experimental Immunology 177, no. 1 (2014):1–12.
- ↩ Martinez, Leone, and Chang, “Western Diets, Gut Dysbiosis, and Metabolic Diseases”; Rook, Raison, and Lowry, “Microbial ‘Old Friends,’ Immunoregulation and Socioeconomic Status.”
- ↩ Nina D’Vaz and Rae-Chi Huang, “Nutrition, Epigenetics and the Early Life Origins of Disease: Evidence from Human Studies,” in Graham Burdge and Karen Lillycrop, eds., Nutrition, Epigenetics and Health (Hackensack: World Scientific, 2016), 25–40; Sathish Subramanian et al., “Cultivating Healthy Growth and Nutrition through the Gut Microbiota,” Cell 161, no. 1 (2015): 36–48.
- ↩ Rook, “Regulation of the Immune System by Biodiversity from the Natural Environment.”
- ↩ Martin J. Blaser and Stanley Falkow, “What Are the Consequences of the Disappearing Human Microbiota?” Nature Reviews Microbiology 7, no. 12 (2009): 887–94; Edward C. Deehan and Jens Walter, “The Fiber Gap and the Disappearing Gut Microbiome: Implications for Human Nutrition,” Trends in Endocrinology & Metabolism 27, no. 5 (2016): 239–42; Sonnenburg et al., “Diet-Induced Extinctions in the Gut Microbiota Compound Over Generations.”
- ↩ Sonnenburg et al., “Diet-Induced Extinctions in the Gut Microbiota Compound Over Generations.”
- ↩ Sonnenburg et al., “Diet-Induced Extinctions in the Gut Microbiota Compound Over Generations.”
- ↩ Michael C. Toh and Emma Allen-Vercoe, “The Human Gut Microbiota with Reference to Autism Spectrum Disorder: Considering the Whole as More than a Sum of Its Parts,” Microbial Ecology in Health and Disease 26 (2015); Rodney R. Dietert and Janice M. Dietert, “The Microbiome and Sustainable Healthcare,” Healthcare 3, no. 1 (2015): 100–29.
- ↩ Ruth E. Ley et al., “Evolution of Mammals and Their Gut Microbes,” Science 320, no. 5883 (2008): 1647–51; Zhenjiang Xu and Rob Knight, “Dietary Effects on Human Gut Microbiome Diversity,” British Journal of Nutrition 113, Supplement 1 (2015): S1–S5.
- ↩ Lindsey G. Albenberg and Gary D. Wu, “Diet and the Intestinal Microbiome: Associations, Functions, and Implications for Health and Disease,” Gastroenterology 146, no. 6 (2014): 1564–72; Aurélie Cotillard et al., “Dietary Intervention Impact on Gut Microbial Gene Richness,” Nature 500, no. 7464 (2013): 585–88; Emmanuelle Le Chatelier et al., “Richness of Human Gut Microbiome Correlates with Metabolic Markers,” Nature 500, no. 7464 (2013): 541–46; Yong, I Contain Multitudes.
- ↩ Cotillard et al., “Dietary Intervention Impact on Gut Microbial Gene Richness”; Le Chatelier et al., “Richness of Human Gut Microbiome Correlates with Metabolic Markers.”
- ↩ Albenberg and Wu, “Diet and the Intestinal Microbiome”; Cotillard et al., “Dietary Intervention Impact on Gut Microbial Gene Richness”; Le Chatelier et al., “Richness of Human Gut Microbiome Correlates with Metabolic Markers.”
- ↩ Albenberg and Wu, “Diet and the Intestinal Microbiome”; Cotillard et al., “Dietary Intervention Impact on Gut Microbial Gene Richness”; Le Chatelier et al., “Richness of Human Gut Microbiome Correlates with Metabolic Markers.”
- ↩ Gary D. Wu and James D. Lewis, “Analysis of the Human Gut Microbiome and Association with Disease,” Clinical Gastroenterology and Hepatology 11, no. 7 (2013): 774–77.
- ↩ Alexander R. Moschen, Verena Wieser, and Herbert Tilg, “Dietary Factors: Major Regulators of the Gut’s Microbiota,” Gut and Liver 6, no. 4 (2012): 411–16; Wu and Lewis, “Analysis of the Human Gut Microbiome and Association with Disease.”
- ↩ Marit K. Zinöcker and Inge A. Lindseth, “The Western Diet–Microbiome-Host Interaction and Its Role in Metabolic Disease,” Nutrients 10, no. 3 (2018): 365.
- ↩ Lawrence A. David et al., “Diet Rapidly and Reproducibly Alters the Human Gut Microbiome,” Nature505, no. 7484 (2014): 559–63.
- ↩ Rachel N. Carmody et al., “Diet Dominates Host Genotype in Shaping the Murine Gut Microbiota,” Cell Host & Microbe 17, no. 1 (2015): 72–84.
- ↩ Jotham Suez, Hagit Shapiro, and Eran Elinav, “Role of the Microbiome in the Normal and Aberrant Glycemic Response,” Clinical Nutrition Experimental 6 (2016): 59–73; Martinez, Leone, and Chang, “Western Diets, Gut Dysbiosis, and Metabolic Diseases.”
- ↩ Ruairi C. Robertson et al., “Omega-3 Polyunsaturated Fatty Acids Critically Regulate Behaviour and Gut Microbiota Development in Adolescence and Adulthood,” Brain, Behavior, and Immunity 59 (2017): 21–37.
- ↩ Kuan-Hsun Huang et al., “Gut Microbiota Increased by Omega-3 Fatty Acids is Negatively Correlated with Hepatic Lipid Metabolism-Associated Genes in mice with High Carbohydrate Diet-Induced Steatosis,” FASEB Journal 31, no. 1 supplement (2017): 654.3; Tali Lanton et al., “SAT-357-Inhibition of IL6 Trans-Signaling Leads to Gut Microbiota-Dependent Mature-Onset Obesity and Metabolic Syndrome,” Journal of Hepatology 66, no. 1 (2017): S609.
- ↩ Yael R. Nobel et al., “Metabolic and Metagenomic Outcomes from Early-Life Pulsed Antibiotic Treatment,” Nature Communications 6 no. 7486 (2015).
- ↩ Blanda Di Luccia et al., “Rescue of Fructose-Induced Metabolic Syndrome by Antibiotics or Faecal Transplantation in a Rat Model of Obesity,” PLoS One 10, no. 8 (2015): e0134893.
- ↩ Fang Liu et al., “Polymannuronic Acid Ameliorated Obesity and Inflammation Associated with a High-Fat and High-Sucrose Diet by Modulating the Gut Microbiome in a Murine Model,” British Journal of Nutrition 117, no. 9 (2017): 1332–42.
- ↩ Benoit Chassaing et al., “How Diet Can Impact Gut Microbiota to Promote or Endanger Health,” Current Opinion in Gastroenterology 33, no. 6 (2017): 417–21.
- ↩ Jun Zou, Benoit Chassaing, and Andrew T. Gewirtz, “Dietary Fiber Protect Against High-Fat Diet-Induced Metabolic Syndrome Through Myd88-Mediated IL-22 Production that Reduces Microbiota Encroachment,” Gastroenterology 152, no. 5 (2017): S1013.
- ↩ Laura V. Blanton et al., “Childhood Undernutrition, the Gut Microbiota, and Microbiota-Directed Therapeutics,” Science 352, no. 6293 (2016): 1533; Mark R. Charbonneau et al., “A Microbial Perspective of Human Developmental Biology,” Nature 535, no. 7610 (2016): 48–55.
- ↩ Blanton et al., “Childhood Undernutrition, the Gut Microbiota, and Microbiota-Directed Therapeutics”; Charbonneau et al., “A Microbial Perspective of Human Developmental Biology.”
- ↩ Blanton et al., “Childhood Undernutrition, the Gut Microbiota, and Microbiota-Directed Therapeutics”; Charbonneau et al., “A Microbial Perspective of Human Developmental Biology.”
- ↩ Blanton et al., “Childhood Undernutrition, the Gut Microbiota, and Microbiota-Directed Therapeutics”; Charbonneau et al., “A Microbial Perspective of Human Developmental Biology.”
- ↩ Blanton et al., “Childhood Undernutrition, the Gut Microbiota, and Microbiota-Directed Therapeutics.”
- ↩ Blanton et al., “Childhood Undernutrition, the Gut Microbiota, and Microbiota-Directed Therapeutics.”
- ↩ Blanton et al., “Childhood Undernutrition, the Gut Microbiota, and Microbiota-Directed Therapeutics.”
- ↩ Martin J. Blaser, “Antibiotic Use and Its Consequences for the Normal Microbiome,” Science 352, no. 6285 (2016): 544–45.
- ↩ Manuel Ferrer et al., “Antibiotic Use and Microbiome Function,” Biochemical Pharmacology 134 (2017): 114–26.
- ↩ Ferrer et al., “Antibiotic Use and Microbiome Function.”
- ↩ Ferrer et al., “Antibiotic Use and Microbiome Function”; Vangay et al., “Antibiotics, Pediatric Dysbiosis, and Disease.”
- ↩ Katri Korpela et al., “Intestinal Microbiome Is Related to Lifetime Antibiotic Use in Finnish Pre-School Children,” Nature Communications 7, no. 10410 (2016).
- ↩ Blaser and Falkow, “What Are the Consequences of the Disappearing Human Microbiota?”
- ↩ Andrew T. Stefka et al., “Commensal Bacteria Protect against Food Allergen Sensitization,” Proceedings of the National Academy of Sciences 111, no. 36 (2014): 13145–50.
- ↩ Katherine King, Kamilla Josefsdottir, and Megan Baldridge, “Antibiotics Impair Murine Hematopoiesis by Depleting Intestinal Microbiota,” Open Forum Infectious Diseases 3, supplement 1 (2016): 2230.
- ↩ Laura M. Cox and Martin J. Blaser, “Antibiotics in Early Life and Obesity,” Nature Reviews Endocrinology 11, no. 3 (2015): 182–90.
- ↩ Britton and Young, “Interaction between the Intestinal Microbiota and Host in Clostridium DifficileColonization Resistance.”
- ↩ Sandrine Isaac et al., “Short- and Long-Term Effects of Oral Vancomycin on the Human Intestinal Microbiota,” Journal of Antimicrobial Chemotherapy 72, no. 1 (2016): 128–36.
- ↩ Inna Sekirov et al., “Antibiotic-Induced Perturbations of the Intestinal Microbiota Alter Host Susceptibility to Enteric Infection,” Infection and Immunity 76, no. 10 (2008): 4726–36; Korpela et al., “Intestinal Microbiome Is Related to Lifetime Antibiotic Use in Finnish Pre-School Children”; Franziska Faber et al., “Host-Mediated Sugar Oxidation Promotes Post-Antibiotic Pathogen Expansion,” Nature534, no. 7609 (2016): 697–99.
- ↩ Keisha Findley et al., “Health Disparities and the Microbiome,” Trends in Microbiology 24, no. 11 (2016): 847–50.
- ↩ Tao Ding and Patrick D. Schloss, “Dynamics and Associations of Microbial Community Types across the Human Body,” Nature 509, no. 7500 (2014): 357–60.
- ↩ Ricardo M. P. de Mello et al., “Lactobacilli and Bifidobacteria in the Feces of Schoolchildren of Two Different Socioeconomic Groups: Children from a Favela and Children from a Private School,” Jornal de Pediatria 85, no. 4 (2009): 307–14.
- ↩ Gregory E. Miller, “Lower Neighborhood Socioeconomic Status Associated with Reduced Diversity of the Colonic Microbiota in Healthy Adults,” PLoS ONE 11, no. 2 (2016): e0148952.
- ↩ Findley et al., “Health Disparities and the Microbiome.”
- ↩ Sachin Goyal et al., “Racial Disparity in Colorectal Cancer: Gut Microbiome and Cancer Stem Cells,” World Journal of Stem Cells 8, no. 9 (2016): 279.
- ↩ Shi Ying et al., “The Influence of Age and Gender on Skin-Associated Microbial Communities in Urban and Rural Human Populations,” PLoS ONE 10, no. 10 (2015): e0141842.
- ↩ Zhenjiang Xu and Rob Knight, “Dietary Effects on Human Gut Microbiome Diversity,” British Journal of Nutrition 113, supplement 1 (2015): S1–S5.
- ↩ Ala Alwan, Global Status Report on Noncommunicable Diseases 2010 (Geneva: World Health Organization, 2010).
- ↩ Anthony Winson, The Industrial Diet: The Degradation of Food and the Struggle for Healthy Eating (New York: New York University Press, 2013).
- ↩ Winson, The Industrial Diet.
- ↩ Loren Cordain et al., “Origins and Evolution of the Western Diet: Health Implications for the 21st Century,” American Journal of Clinical Nutrition 81, no. 2 (2005): 341–54.
- ↩ Winson, The Industrial Diet.
- ↩ Winson, The Industrial Diet.
- ↩ Cordain et al., “Origins and Evolution of the Western Diet”; Winson, The Industrial Diet.
- ↩ Cordain et al., “Origins and Evolution of the Western Diet”; Winson, The Industrial Diet.
- ↩ Winson, The Industrial Diet.
- ↩ Winson, The Industrial Diet.
- ↩ Winson, The Industrial Diet.
- ↩ Cristin E. Kearns, Laura A. Schmidt, and Stanton A. Glantz, “Sugar Industry and Coronary Heart Disease Research: A Historical Analysis of Internal Industry Documents,” JAMA Internal Medicine 176, no. 11 (2016): 1680–85; Winson, The Industrial Diet.
- ↩ Winson, The Industrial Diet.
- ↩ Winson, The Industrial Diet.
- ↩ Winson, The Industrial Diet.
- ↩ Winson, The Industrial Diet.
- ↩ Winson, The Industrial Diet.
- ↩ Winson, The Industrial Diet.
- ↩ Elizabeth Black, “Globalization of the Food Industry: Transnational Food Corporations, the Spread of Processed Food, and Their Implications for Food Security and Nutrition,” School of International Training Switzerland (2016).
- ↩ Black, “Globalization of the Food Industry.”
- ↩ Winson, The Industrial Diet.
- ↩ Winson, The Industrial Diet.
- ↩ Black, “Globalization of the Food Industry.”
- ↩ Black, “Globalization of the Food Industry.”
- ↩ Black, “Globalization of the Food Industry.”
- ↩ Winson, The Industrial Diet.
- ↩ Winson, The Industrial Diet.
- ↩ Winson, The Industrial Diet.
- ↩ Winson, The Industrial Diet.
- ↩ Winson, The Industrial Diet.
- ↩ Shannon N. Zenk et al., “Neighborhood Racial Composition, Neighborhood Poverty, and the Spatial Accessibility of Supermarkets in Metropolitan Detroit,” American Journal of Public Health 95, no. 4 (2005): 660–67; Peter Riley Bahr, “Race and Nutrition: An Investigation of Black–White Differences in Health-Related Nutritional Behaviours,” Sociology of Health & Illness 29, no. 6 (2007): 831–56; David Himmelgreen et al., “‘I Don’t Make the Soups Anymore’: Pre- to Post-Migration Dietary and Lifestyle Changes Among Latinos Living in West-Central Florida,” Ecology of Food and Nutrition 46, nos. 5–6 (2007): 427–44; Nicole Darmon and Adam Drewnowski, “Does Social Class Predict Diet Quality?” American Journal of Clinical Nutrition 87, no. 5 (2008): 1107–17; Adam Drewnowski, “Obesity, Diets, and Social Inequalities,” Nutrition Reviews 67, supplement 1 (2009): S36–S39; Marilda Borges Neutzling et al., “Factors Associated with Fruit and Vegetable Intake among Adults in a Southern Brazilian City,” Cadernos de Saudepublica 25, no. 11 (2009) 2365–74; Anju Aggarwal et al., “Does Diet Cost Mediate the Relation between Socioeconomic Position and Diet Quality?” European Journal of Clinical Nutrition 65, no. 9 (2011): 1059–66.
- ↩ Geoffrey Rose and M. G. Marmot, “Social Class and Coronary Heart Disease,” Heart 45, no. 1 (1981): 13–19; Steven Cummins and Sally Macintyre, “Food Environments and Obesity—Neighbourhood or Nation?” International Journal of Epidemiology 35, no. 1 (2006): 100–04; Julie Guthman and Melanie DuPuis, “Embodying Neoliberalism: Economy, Culture, and the Politics of Fat,” Environment and Planning D: Society and Space 24, no. 3 (2006): 427–48; John Sankofa and Wendy L. Johnson-Taylor, “News Coverage of Diet-Related Health Disparities Experienced by Black Americans: A Steady Diet of Misinformation,” Journal of Nutrition Education and Behavior 39, no. 2 (2007): S41–S44; Sonia Caprio et al., “Influence of Race, Ethnicity, and Culture on Childhood Obesity: Implications for Prevention and Treatment,” Diabetes Care 16, no. 12 (2008): 2566–77; Roni A. Neff, “Food Systems and Public Health Disparities,” Journal of Hunger & Environmental Nutrition 4, nos. 3–4 (2009): 282–314; Carolyn C. Cannuscio, Eve E. Weiss, and David A Asch, “The Contribution of Urban Food Ways to Health Disparities,” Journal of Urban Health 87, no. 3 (2010): 381–93; Tonya Moore, “Socioeconomic Patterning of Obesity among African American Women in the Jackson Heart Study” (PhD diss., University of Alabama at Birmingham, 2012).
- ↩ Rob Wallace, Big Farms Make Big Flu (New York: Monthly Review Press, 2016).
- ↩ Thomas P. Van Boeckel et al., “Global Antibiotic Consumption 2000 to 2010: An Analysis of National Pharmaceutical Sales Data,” Lancet Infectious Diseases 14, no. 8 (2010): 742–50.
- ↩ Harry Björklund, Johan Bondestam, and Göran Bylund, “Residues of Oxytetracycline in Wild Fish and Sediments from Fish Farms,” Aquaculture 86, no. 4 (1990): 359–67; Laura M. Cox and Martin J. Blaser, “Antibiotics in Early Life and Obesity,” Nature Reviews Endocrinology 11, no. 3 (2015): 182–90; Wageh Sobhy Darwish et al., “Antibiotic Residues in Food: The African Scenario,” Japanese Journal of Veterinary Research 61, supplement (2013): S13–S22; Dan J. Donoghue, “Antibiotic Residues In Poultry Tissues and Eggs: Human Health Concerns?” Poultry Science 82, no. 4 (2003): 618–21; Sapna Johnson and Nimisha Jadon, “Antibiotic Residues in Honey,” Centre for Science and Environment, 2010; Seyda Ergin Kaya and Ayhan Filazi, “Determination of Antibiotic Residues in Milk Samples,” Kafkas Universitesi Veteriner Fakultesi Dergisi 16, supplement A (2010): S31–S35; Wim Reybroeck, “Residues of Antibiotics and Sulphonamides in Honey on the Belgian Market,” Apiacta 38 (2003): 23–30; Miho Yamaki et al., “Occurrence of Antibiotic Residues in Milk from Manchega Ewe Dairy Farms,” Journal of Dairy Science 87, no. 10 (2004): 3132–37.
- ↩ Richard Anderson, “Pharmaceutical Industry Gets High on Fat Profits,” BBC News, November 6, 2014; Akshat Rathi, “To Fight Antibiotic Resistance, We May Have to Pay the Hugely Profitable Pharma Industry Even More,” Quartz, May 20, 2015, http://qz.com.
- ↩ Bashar Hamad, “The Antibiotics Market,” Nature Reviews Drug Discovery 9, no. 9 (2010): 675–76.
- ↩ “Antibacterial Drugs Market (By Class —Aminoglycosides, B-Lactams, Tetracyclines, Sulfonamides, Quinolones/ Fluoroquinolones, Macrolides and Phenicols, and Pipeline Analysis)—Global Industry Analysis, Size, Share, Growth, Trends and Forecast, 2013–2019,” Transparency Market Research, March 2014.
- ↩ Hellen Gelbland et al., The State of the World’s Antibiotics 2015 (Washington, D.C.: Center for Disease Dynamics, Economics and Policy, 2015).
- ↩ Maryn McKenna, “We Need Antibiotics. They’re Not Profitable To Make. Who Pays?” National Geographic Germination blog, May 23, 2015, http://phenomena.nationalgeographic.com; Rathi, “To Fight Antibiotic Resistance, We May Have to Pay the Hugely Profitable Pharma Industry Even More.”
- ↩ William Greene, “The Emergence of India’s Pharmaceutical Industry and Implications for the U.S. Generic Drug Market,” U.S. International Trade Commission Office of Economics Working Paper, May 2007, http://usitc.gov; Gardiner Harris, “Drug Making’s Move Abroad Stirs Concerns,” New York Times, January 19, 2009.
- ↩ Roger Finch, “Generic Antibiotics, Antibiotic Resistance, and Drug Licensing,” Lancet Infectious Diseases 10, no. 11 (2010): 754.
- ↩ Patricia Van Arnum, “The Weaknesses and Strengths of the Global API Market,” Pharmaceutical Technology Sourcing and Management 9, no. 3 (2013); “Antibacterial Drugs Market.”
- ↩ Bad Medicine: How the Pharmaceutical Industry Is Contributing to the Global Rise of Antibiotic-Resistant Superbugs (New York: SumOfUs, 2015).
- ↩ Pierre-Louis Toutain and Alain Bousquet-Melou, “The Consequences of Generic Marketing on Antibiotic Consumption and the Spread of Microbial Resistance: The Need for New Antibiotics,” Journal of Veterinary Pharmacology and Therapeutics 36, no. 5 (2013): 420–24.
- ↩ Van Boeckel et al., “Global Antibiotic Consumption 2000 to 2010.”
- ↩ Van Boeckel et al., “Global Antibiotic Consumption 2000 to 2010.”
- ↩ Van Boeckel et al., “Global Antibiotic Consumption 2000 to 2010.”
- ↩ Nobel et al., “Metabolic and Metagenomic Outcomes from Early-Life Pulsed Antibiotic Treatment.”
- ↩ Ramanan Laxminarayan et al., “Access to Effective Antimicrobials: A Worldwide Challenge,” Lancet387, no. 10014 (2015): 168–75.
- ↩ Gelbland et al., The State of the World’s Antibiotics 2015.
- ↩ Gelbland et al., The State of the World’s Antibiotics 2015.
- ↩ Joan Busfield, “‘A Pill for Every Ill’: Explaining the Expansion in Medicine Use,” Social Science & Medicine 70, no. 6 (2010): 934–41.
- ↩ Busfield, “‘A Pill for Every Ill'”; Joan Busfield, “Assessing the Overuse of Medicines,” Social Science & Medicine 131 (2014): 1–8.
- ↩ John Abraham, “Pharmaceuticalization of Society in Context: Theoretical, Empirical and Health Dimensions,” Sociology 44, no. 4 (2010): 603–22; Busfield, “‘A Pill for Every Ill.'”
- ↩ Abraham, “Pharmaceuticalization of Society in Context.”
- ↩ Busfield, “‘A Pill for Every Ill'”; Simon J. Williams, Paul Martin, and Jonathan Gabe, “The Pharmaceuticalisation of Society? A Framework for Analysis,” Sociology of Health & Illness 33, no. 5 (2011): 710–25.
- ↩ Abraham, “Pharmaceuticalization of Society in Context.”
- ↩ Abraham, “Pharmaceuticalization of Society in Context.”
- ↩ Abraham, “Pharmaceuticalization of Society in Context.”
- ↩ Busfield, “‘A Pill for Every Ill.'”
- ↩ Abraham, “Pharmaceuticalization of Society in Context.”
- ↩ Elizabeth Siegel Watkins, “Technophilia and the Pharmaceutical Fix,” Lancet 376, no. 9753 (2010): 1638–39.
- ↩ Busfield, “Assessing the Overuse of Medicines.”
- ↩ Busfield, “‘A Pill for Every Ill.'”
- ↩ Busfield, “‘A Pill for Every Ill'”; Abraham, “Pharmaceuticalization of Society in Context.”
- ↩ Busfield, “‘A Pill for Every Ill.'”
- ↩ Busfield, “‘A Pill for Every Ill.'”
- ↩ Watkins, “Technophilia and the Pharmaceutical Fix.”
- ↩ Watkins, “Technophilia and the Pharmaceutical Fix.”
- ↩ Jill A. Fisher, “Coming Soon to a Physician Near You: Medical Neoliberalism and Pharmaceutical Clinical Trials,” Harvard Health Policy Review 8, no. 1 (2007): 61–70.
- ↩ Fisher, “Coming Soon to a Physician Near You.”
- ↩ Williams, Martin, and Gabe, “The Pharmaceuticalisation of Society?”
- ↩ John Abraham, “The Pharmaceutical Industry as a Political Player,” Lancet 360, no. 9344 (2002): 1498–1502; Rebeca Jasso-Aguilar and Howard Waitzkin, “Multinational Corporations, the State, and Contemporary Medicine,” Health Sociology Review 20, no. 3 (2011): 245–57; Williams, Martin, and Gabe, “The Pharmaceuticalisation of Society?”
- ↩ Abraham, “The Pharmaceutical Industry as a Political Player”; Jasso-Aguilar and Waitzkin, “Multinational Corporations, the State, and Contemporary Medicine”; Williams, Martin, and Gabe, “The Pharmaceuticalisation of Society?”; Zahra Meghani and Jennifer Kuzma, “The ‘Revolving Door’ between Regulatory Agencies and Industry: A Problem That Requires Reconceptualizing Objectivity,” Journal of Agricultural and Environmental Ethics 24, no. 6 (2011): 575–99.
- ↩ Abraham, “Pharmaceuticalization of Society in Context.”
- ↩ Yong, I Contain Multitudes.
- ↩ Alan C. Logan, Felice N. Jacka, and Susan L. Prescott, “Immune-Microbiota Interactions: Dysbiosis as a Global Health Issue,” Current Allergy and Asthma Reports 16, no. 2 (2016): 13.
- ↩ Langdon, Crook, and Dantas, “The Effects of Antibiotics on the Microbiome throughout Development and Alternative Approaches for Therapeutic Modulation”; Jee Loon Foo et al., “Microbiome Engineering: Current Applications and Its Future,” Biotechnology Journal 12, no. 3 (2017).
- ↩ Dominique L. Monnet, “Antibiotic Development and the Changing Role of the Pharmaceutical Industry,” International Journal of Risk & Safety in Medicine 17, nos. 3–4 (2005): 133–45; Chantal M. Morel and Elias Mossialos, “Stoking the Antibiotic Pipeline,” British Medical Journal 340 (2010): 1115–18.
No comments:
Post a Comment